
Management of failed autogenous tissues temporomandibular joint reconstruction: case series and literature review
Highlight box
Key findings
• Patients with a diagnosis of TMJ disorders who underwent Temporomandibolar Joint Reconstruction at the Division Maxillofacial Surgery, Città della Salute e della Scienza University Hospital, University of Torino, between January 2001 and September 2021 were retrospectively analyzed. This retrospective analysis enrolled 20 patients who underwent prosthesis TMJR with previous autogenous graft. Ankylosis recurred in 4 patients and 1 patient had infection and 1 had necrosis. 4 patients have undergone further surgery including 1 resurfacing (cleavage or soft tissue graft), 3 graft removal and, finally, in all cases total alloplastic joint replacement was performed
What is known and what is new?
• Traditional reconstruction methods based on the use of local osteotomy, distraction osteogenesis, bone graft with non-vascularized tissue (costochondral, sternoclavicular) or vascularized tissue (second metatarsal, fibula) with the eventual interposition of soft tissue (mainly temporal fascia flap) are still used by experienced surgeon and in low income country, delivering good results.
• The rate of failure of autogenous tissue, specially for the very popular rib grafts is not negligeable and in this scenarios reconstruction of TMJ is a difficult challenge.
• In this manuscript we demonstrated that the failure of autogenous tissue reconstruction of TMJ is the main indications for total alloplastic TMJ reconstruction.
What is the implication, and what should change now?
• The implication and the novelty that this study introduces is to demonstrate that when patients have undergone previous TMJ replacement operations with autogenous tissues and these have failed, the TMJ prosthesis is the best choice to provide functional results and predictable morphology.
Introduction
Alloplastic temporomandibular joint (TMJ) total reconstruction is considered an effective procedure for the treatment of end stage TMJ conditions with stable results (1-4).
Short, medium and long term (up to 20 years) outcome studies suggest that total TMJ alloplastic reconstruction provides predictable and long standing results in terms of reduction of pain, improvement of mandibular function and shape, improvement of diet consistency and quality of life scores (4-7).
Reduction of operating time, early mobilization and avoidance of donor site morbidity are well known advantages of alloplastic total joint replacement (TJR) over conventional reconstruction with autogenous graft.
In the majority of high income countries with advanced health care systems, TMJ prosthetic total reconstruction represents the first choice procedure to manage TMJ end-stage joint disease (8,9).
Traditional reconstruction methods based on the use of local osteotomy, distraction osteogenesis, bone graft with non-vascularized tissue (costochondral, sternoclavicular) or vascularized tissue (second metatarsal, fibula) with the eventual interposition of soft tissue (mainly temporal fascia flap) are still used by experienced surgeon and in low income country, delivering good results.
Many studies have focused on the pro and drawbacks of traditional methods (10,11). The rate of failure of autogenous tissue, specially for the very popular rib grafts is not negligeable and in this scenarios reconstruction of TMJ is a difficult challenge (12-16).
The American Association of Oral and Maxillofacial Surgeons (AAOMS) and the guidelines of the UK National Institute for Health and Care Excellence report the following indications for total TMJ alloplastic reconstruction: (I) TMJ operated in multiple ways with inadequate results; (II) ongoing symptoms and severe functional limitations despite previous alloplastic implants; (III) autoimmune diseases and connective tissues; (IV) inflammatory, infectious or reactive diseases; (V) ankylosis; (VI) failed reconstruction with autogenous grafts; (VII) neoplasm.
The purpose of this article is to report the University of Torino experience and to review the literature on the on the management of failed autogenous tissues using TMJ prosthesis. We present this article in accordance with the AME Case Series reporting checklist and the Narrative Review reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-28/rc).
Case presentation
Torino experience
Patients with a diagnosis of TMJ disorders (TMDs) who underwent TMJ replacement (TMJR) at the Division Maxillofacial Surgery, Città della Salute e della Scienza University Hospital, University of Torino, between January 2001 and September 2021 were retrospectively analyzed.
The inclusion criteria were as follow: previous autogenous graft in the TMJ region; previous reconstruction of condyle-ramus unit by mean of distraction osteogenesis or local osteotomies; complete and adequate pre and postoperative follow up clinical records; computed tomography (CT) and magnetic resonance imaging (MRI) pre-op, immediately postoperative and at the longest follow up; follow up of at least 12 months.
Exclusion criteria were incomplete clinical and radiological records.
Data were collected 1 month preoperatively (T0) and at the longest follow up (T1). Objective parameters measured at T0 and T1 included maximum interincisal opening (MIO), measured clinically with a metric ruler in millimeters.
Demographics, patient features and follow up period are summarized in Tables 1,2.
Table 1
| Patient | Sex (F/M) |
Diagnosis | Joint/s | Type | Previous surgery | Further surgery | Follow up (months) |
|---|---|---|---|---|---|---|---|
| 1 | F | Ankylosis post perinatal infection | L | Stock | CCG | – | 212 |
| 2 | M | Ankylosis post perinatal infection | R | Stock | CCG | Resurfacing | 180 |
| 3 | M | Ankylosis post perinatal infection | B | Stock | CCG | – | 120 |
| 4 | F | Ankylosis post perinatal infection | B | Stock | CCG | – | 108 |
| 5 | F | Ankylosis post perinatal infection | B | Custom | CCG | Osteogenesis distraction | 96 |
| 6 | M | Ankylosis associated with Goldenhar syndrome | B | Custom | CCG | – | 96 |
| 7 | M | Ankylosis post perinatal infection | B | Custom | CCG | – | 84 |
| 8 | M | Ankylosis post perinatal infection | R | Custom | CCG | Resurfacing | 84 |
| 9 | F | Ankylosis post perinatal infection | R | Custom | CCG | Graft removal | 78 |
| 10 | F | Ankylosis associated with Apert syndrome | B | Custom | DO | – | 78 |
| 11 | F | Ankylosis post perinatal infection | B | Custom | CCG | – | 78 |
| 12 | M | Ankylosis post perinatal infection | L | Custom | CCG | Graft removal | 120 |
| 13 | M | Ankylosis post perinatal infection | B | Custom | CCG | – | 78 |
| 14 | M | Ankylosis post perinatal infection | L | Custom | CCG | Graft removal | 12 |
| 15 | M | Ankylosis associated with Goldenhar syndrome | B | Custom | CCG | – | 12 |
| 16 | F | Ankylosis post perinatal infection | B | Custom | CCG | Osteogenesis distraction | 108 |
| 17 | F | Ankylosis post perinatal infection | L | Custom | DO | Resurfacing | 12 |
F, female; M, male; B, bilateral; L, left; R, right; CCG, cocostocondral graft; DO, distraction osteogenesis; TMJ, temporolmandibular joint.
Table 2
| Patient | Sex (F/M) | Diagnosis | Joint/s | Type | Previous surgery | Further surgery | Follow up |
|---|---|---|---|---|---|---|---|
| 1 | F | Ameloblastoma | L | Custom | CCG | – | 207 |
| 2 | M | Ameloblastoma | R | Custom | Lliac crest bone graft | – | 108 |
| 3 | M | Ameloblastoma | R | Custom | Fibula free flap | – | 113 |
F, female; M, male; B, bilateral; L, left; R, right; CCG, cocostocondral graft.
Subjective variables included: 1) TMJ pain (0 = no pain, 10 = severe pain 2), diet (0 = normal diet, 10 = only liquid diet) and quality of life (QoL) pre and after treatment was measured on an ordinary Visual Analogous Scale (VAS) 10-point scale, ranging from 0 (much worse) to 10 (much better) (Tables 3,4).
Table 3
| Variables | Degree | Score |
|---|---|---|
| TMJ pain | “No” to “Worse” | 0 to 10 |
| Diet | “No restriction” to “Liquid” | 0 to 10 |
| QoL | “Improve” to “Worse” | 0 to 10 |
The subjective assessment used the following questions. The variables were rated on a scale of 0–10. QoL, quality of life; TMJ, temporomandibular joint.
Table 4
| Measurement | Preoperative (median) | Postoperative (median) |
|---|---|---|
| MIO, mm | 5.4 | 27.8 |
| TMJ pain | 7 | 4.2 |
| Diet | 8.3 | 3.4 |
| QoL | 8.2 | 3.6 |
MIO, maximum interincisival opening; TMJ, temporomandibular joint; QoL, quality of life.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Literature review
A computerized literature review was performed in accordance with PRISMA statement (Preferred Reporting Items for Systematic Reviews an Meta-Analyzes).
The following search terms were used: (TMJ replacement or Temporomandibular joint) AND (autogenous tissues) or AND (costochondral Grafts) or (Vascularized costochondral Grafts) AND (Sternoclavicular graft) or AND (Fibula graft) AND (autogenous tissues failed).
The aim of the review was to analyze the effectiveness and indications of the total alloplastic TMJ replacement in case of the autogenous tissue were failed.
We only considered replacement surgery with autogenous tissues: costochondral Graft, Sternoclavicular graft, and fibula graft.
The search strategy was performed to locate all pertinent articles published from January 2000 to January 2022.
The following inclusion criteria were adopted based on the PICOS (patient, intervention, comparison, outcomes, study design)—P: patients were undergoing total alloplastic TMJ replacement; I: previous surgery; C: replacement with autogenous tissues failed vs. replacement with autogenous tissues; O: MIO and in post operative (follow up minimum 12 months); S: study design: controlled trials, retrospective studies, case series and prospective with the aim of evaluating the management of failed autogenous tissues using TMJ prostheses.
The following exclusion criteria were applied: animals trials.
Results
Torino experience
This retrospective analysis enrolled 17 (9 male, 7 female) patients who underwent TMJ reconstruction with previous costochondral graft and 3 patients (2 male and 1 female) with previous reconstruction of condyle and mandible by autogenous grafts or local osteotomies at the Division of Maxillofacial Surgery, Città della Salute e della Scienza University Hospital, University of Torino, between January 2001 and September 2021. The average follow up was 112 months (range, 12–212 months).
For 17 patients, initial diagnosis was congenital ankylosis as a sequela of local perinatal infection or associated with congenital syndrome, for three patients the initial diagnosis was ameloblastoma.
Thus, we analyzed the results by dividing the patients in two subgroups: group A recurrent of congenital ankylosis after rib graft or distraction osteogenesis (DO), group B failure of mandibular reconstruction.
Group A
The seventeen patients with initial diagnosis of ankylosis underwent autogenous tissue reconstruction in other institutions; ankylosis recurred in all these patients. Eight patients further underwent surgery including: 3 resurfacing of the graft with temporals fascia, 3 graft removal and 2 osteogenesis distraction (Figure 1).
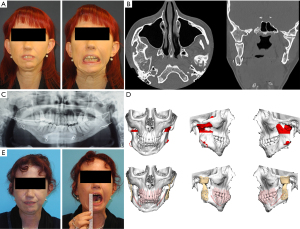
Six patients underwent Zimmer/Biomet (Jacksonville, FL, USA) total joint reconstruction system with stock prosthesis (4 bilateral and 2 monolateral); 11 patients underwent total joint reconstruction system with custom-made devices: 7 Biomet, 2 TMJ Concept (Ventura, CA, USA) and 2 Cadskills (Gent, Belgium, EU) (6 bilateral, 5 monolateral). In 5 patients the jaw was repositioned with mandibular advancement supported by the custom prosthesis with the concomitant reposition of the maxilla.
Preoperative MIO was 5.4 mm and postoperative MIO was 27.8 mm.
In one case we registered an early post operative periprosthetic joint infection. The complication was successfully managed with surgical debridement and prolonged antibiotics with device retention according to Wolford protocol (17) (40 month follow up). No ankylosis relapse was registered.
Data were summarized in Table 1.
Group B
In the 3 patients with initial diagnosis of ameloblastoma the ramus-condyle unit was previously reconstructed in 1 case with iliac crest bone graft, 1 case CGC graft and 1 with fibula free flap (Figure 2).
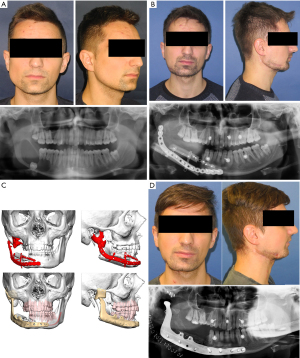
All the cases were unilateral and reconstructed with custom devices: 2 Biomet, 1 TMJ Concept. One case has a slide malocclusion and was managed with dental rehabilitation.
The reasons for failure of autogenous tissue reconstruction were: 1 case infection and osteosynthesis failure, 1 case osteoarthrosis and 1 case necrosis.
Data are summarized in Table 2.
Literature review
The initial screening yielded a total of 45 articles. To analyze results we decided to consider only the articles that focused on the management of failed autogenous tissues in the TMJR. Several studies were published on the TMJ reconstruction with autogenous tissues, in contrast not many publications were found on the management of failed autogenous tissue.
We finally considered 6 articles. We found 1 case report (17), 3 retrospective reviews (11,14,18), 2 retrospective studies (13,19).
These studies compared the use of autogenous tissue and alloplastic reconstruction in terms of improving pain relief, joint function and donor site morbidity. All the clinical studies of this review have shown that alloplastic total reconstruction is a noticeable option when autogenous tissue failed.
Discussion
The use of autogenous tissue, in particular costochondral graft (CCG), has been reported in previous years as gold standard for TMJ reconstruction in the growing patient (20,21).
CCG has been the most commonly used autogenous graft. The main reason to use CCG are the potential growth in pediatric patients and the anatomical features mimicking the condylar form. The CCG can be harvested with a sufficient length for bilateral condyle ramus-unit reconstruction allowing increase of the posterior facial height. Fibula, metatarsal, cranium, clavicle, and iliac crest are the other autogenous grafts reported in literature.
Nevertheless, the literature reports some cons of CCG, like potentials pneumothorax, rib fracture, reankylosis and unpredictable growth with potential overgrowth or graft resorption (21,22).
In skeletally immature patients with residual potential growth the costochondral graft has been considered the gold standard for a long time, but recurrent ankylosis due to overgrowth and heterotopic bone formation has been frequently reported (23).
Ohara et al. (22) reports a 20% rate of residual rib deformity when grafts were harvested from patients older than 10 years but 63% in patients younger than 10 years, leading to chest wall deformities and thoracic scoliosis.
Complications are not negligeable with CCG, as showed by Awal et al. (24). In a 10 year follow up 58.2% of patients suffered at least one complication with ankylosis (32.7%) and overgrowth (16.4%) being the most common. Kumar (23) concluded that the growth potential reported with CCG lacks scientific evidence.
Chen et al. (25) reported a recurrence rate for ankylosis of 19.1% in children and of 7.3% in adults. Stratifying the patient according to the reconstruction method, in children there was not statistical difference between distraction osteogenesis and CCG, while in adults the highest rate of recurrence was associated with reconstruction performed with coronoid process graft (26.4%) in comparison with a 0% rate with TMJ prosthesis implantation.
In children, the current preference is for autogenous reconstruction which can potentially “grow” with the child. The current debate focuses on the possibility of alloplastic reconstruction, particularly where autogenous tissue has failed. The balance seems to swing towards alloplastic reconstruction in adolescents, older children and in extremely complex cases, burdened by multiple failures and recurrent relapses following reconstruction with traditional methods. Consensus and evidence on this topic are still lacking due to small numbers of cases and incomplete long term follow up (26,27).
In adult patients, the failure of autogenous tissues reconstruction is reported as one of the main indication for total alloplastic TMJ reconstruction (12-15).
In the case series presented in this study, we treated 15 patients of different ages with reankylosis following a rib graft performed in other hospitals. In all these cases, the treatment was resolutive and we did not observe any recurrence of ankylosis, with a long term follow up, up to 18 years in the oldest case.
In a previous study, the same authors of this paper suggested a reduced rate of ankylosis recurrence with the use of TMJ alloplastic devices (15,28). Time and longer follow up strengthens our considerations:
- Radical resection of the ankylosis. The insetting of total TMJ reconstruction device requests space in height and in lateral to medial direction at the level of the glenoid fossa, leading the surgeon to remove completely the ankylotic block.
- Coronoidectomy.
- Stage resection and total alloplastic joint reconstruction. Immediate postoperative mobilization and jaw opening exercises are possible and strongly suggested. Westermark advocated that early start of intensive post-operative physiotherapy has to last at least for 1 year and ideally continued life long (15,29).
Considering the MIO results it must be considered that previous surgeries and long standing ankylosis generates a lot of scar in the periarticular soft tissues. This, as stated by Westermark and Aagard, reduces the stretching capabilities of all surrounding tissue components (29,30) making unrealistic to restore a full range of motion of the jaws. Thus, a MIO greater than 25 mm and maintained permanently without recurrence of ankylosis could be considered a satisfactory clinical outcome (3) than 25 mm and maintained permanently could be considered a success (3). It must be stretched the importance of prolonged physiotherapy.
Mercuri (3) reported that capillaries can penetrate a maximum tissue thickness of 180 to 220 mm, whereas scar tissue surrounding previously operated bone averages a thickness of 440 mm. This condition may lead to the clinical observation of increased rate of failure of free autogenous bone grafts in multiply operated patients and in patient with considerable anatomical alteration because of severe pathologies. or pathologies.
In case of failure of an autogenous graft, the recipient bed has poor vascularization, indicating the need for the use of vascularized graft or alloplast (13).
In recent years, in case of failure of previous autogenous reconstruction of segmental defect of mandible including the TMJ, the use of extended TMJ TJR alloplastic devices has been advocated by different authors with promising results (9,31-33). In our series we report three cases of failed autogenous tissue reconstruction repaired with the use of extended total alloplastic TMJ reconstruction.
In selected patients, in case of failure of autogenous grafts, the use of an alloplastic extended TMJ device decreases morbidity, avoids donor site morbidity and reduces operating time in comparison to vascularized graft which are the common choice in this scenario.
There are no studies published in the literature specifically addressing the treatment of patient with failed autogenous reconstruction of the TMJ.
Nevertheless, even if there is no study on this topic with high level of evidence, in all the studies coming from high volume centre (13,32-35), the failure of autogenous tissue reconstruction of TMJ is mentioned among the main indications for total alloplastic TMJ reconstruction.
In this specific group of patients, the distorted or missing anatomy strongly suggest the use of patient specific custom devices.
Conclusions
In conclusion, according to the results of the presented case series and the experts opinions available in literature, when patients have undergone previous TMJ replacement operations with autogenous tissues and these have failed, TMJR prosthesis is the best choice to provide predictable functional and morphologic outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Louis Mercuri) for the series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the AME Case Series reporting checklist and the Narrative Review reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-28/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-28/coif). The series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication of this case series and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Giannakopoulos HE, Sinn DP, Quinn PD. Biomet Microfixation Temporomandibular Joint Replacement System: a 3-year follow-up study of patients treated during 1995 to 2005. J Oral Maxillofac Surg 2012;70:787-94; discussion 795-6. [Crossref] [PubMed]
- Mercuri LG, Caicedo MS. Material Hypersensitivity and Alloplastic Temporomandibular Joint Replacement. J Oral Maxillofac Surg 2019;77:1371-6. [Crossref] [PubMed]
- Mercuri LG. Temporomandibular Joint Total Joint Replacement – TMJ TJR: A Comprehensive Reference for Researchers, Material Scientists and Surgeons. New York: Springer International Publishing, 2015.
- Mercuri LG, Giobbie-Hurder A. Long-term outcomes after total alloplastic temporomandibular joint reconstruction following exposure to failed materials. J Oral Maxillofac Surg 2004;62:1088-96. [Crossref] [PubMed]
- Sidebottom AJ. Reconstruction of the temporomandibular joint in adults and children. J Oral Biol Craniofac Res 2021;11:476-7. [Crossref] [PubMed]
- Gerbino G, Zavattero E, Bosco G, et al. Temporomandibular joint reconstruction with stock and custom-made devices: Indications and results of a 14-year experience. J Craniomaxillofac Surg 2017;45:1710-5. [Crossref] [PubMed]
- Wolford LM, Mercuri LG, Schneiderman ED, et al. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg 2015;73:952-60. [Crossref] [PubMed]
- Dimitroulis G. Management of temporomandibular joint disorders: A surgeon's perspective. Aust Dent J 2018;63:S79-90. [Crossref] [PubMed]
- Elledge R, Mercuri LG, Attard A, et al. Review of emerging temporomandibular joint total joint replacement systems. Br J Oral Maxillofac Surg 2019;57:722-8. [Crossref] [PubMed]
- Awal DH, Jaffer M, Charan G, et al. Costochondral grafting for paediatric temporomandibular joint reconstruction: 10-year outcomes in 55 cases. Int J Oral Maxillofac Surg 2018;47:1433-8. [Crossref] [PubMed]
- Saeed NR, Kent JN. A retrospective study of the costochondral graft in TMJ reconstruction. Int J Oral Maxillofac Surg 2003;32:606-9. [Crossref] [PubMed]
- Johnson NR, Roberts MJ, Doi SA, et al. Total temporomandibular joint replacement prostheses: a systematic review and bias-adjusted meta-analysis. Int J Oral Maxillofac Surg 2017;46:86-92. [Crossref] [PubMed]
- Sidebottom AJ. Alloplastic or autogenous reconstruction of the TMJ. J Oral Biol Craniofac Res 2013;3:135-9. [Crossref] [PubMed]
- Mercuri LG, Ali FA, Woolson R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of reankylosis of the temporomandibular joint. J Oral Maxillofac Surg 2008;66:1794-803. [Crossref] [PubMed]
- Wolford LM, Rodrigues DB, McPhillips A. Management of the infected temporomandibular joint total joint prosthesis. J Oral Maxillofac Surg 2010;68:2810-23. [Crossref] [PubMed]
- Cascone P, Basile E, Angeletti D, et al. TMJ replacement utilizing patient-fitted TMJ TJR devices in a re-ankylosis child. J Craniomaxillofac Surg 2016;44:493-9. [Crossref] [PubMed]
- Bhardwaj Y, Arya S. Post-Ankylotic Temporomandibular Joint Reconstruction Using Autogenous/Alloplastic Materials: Our Protocol and Treatment Outcomes in 22 Patients. Craniomaxillofac Trauma Reconstr 2016;9:284-93. [Crossref] [PubMed]
- Movahed R, Mercuri LG. Management of temporomandibular joint ankylosis. Oral Maxillofac Surg Clin North Am 2015;27:27-35. [Crossref] [PubMed]
- Taylor RC, Ware WH, Horowitz MJ. The importance of determining the end point in treatment of patients with temporomandibular joint syndrome. J Oral Med 1967;22:3-6. [PubMed]
- Poswillo D. Conservative management of degenerative temporomandibular joint disease in the elderly. Int Dent J 1983;33:325-31. [PubMed]
- Hawkins A, Mercuri LG, Miloro M. Are Rib Grafts Still Used for Temporomandibular Joint Reconstruction? J Oral Maxillofac Surg 2020;78:195-202. [Crossref] [PubMed]
- Ohara K, Nakamura K, Ohta E. Chest wall deformities and thoracic scoliosis after costal cartilage graft harvesting. Plast Reconstr Surg 1997;99:1030-6. [Crossref] [PubMed]
- Kumar P, Rattan V, Rai S. Do costochondral grafts have any growth potential in temporomandibular joint surgery? A systematic review. J Oral Biol Craniofac Res 2015;5:198-202. [Crossref] [PubMed]
- Mittal N, Goyal M, Sardana D. Autogenous grafts for reconstruction arthroplasty in temporomandibular joint ankylosis: a systematic review and meta-analysis. Br J Oral Maxillofac Surg 2022;60:1151-8. [Crossref] [PubMed]
- Chen S, He Y, An JG, et al. Recurrence-Related Factors of Temporomandibular Joint Ankylosis: A 10-Year Experience. J Oral Maxillofac Surg 2019;77:2512-21. [Crossref] [PubMed]
- Mercuri LG, Swift JQ. Considerations for the use of alloplastic temporomandibular joint replacement in the growing patient. J Oral Maxillofac Surg 2009;67:1979-90. [Crossref] [PubMed]
- Sinn DP, Tandon R, Tiwana PS. Can Alloplastic Total Temporomandibular Joint Reconstruction be Used in the Growing Patient? A Preliminary Report. J Oral Maxillofac Surg 2021;79:2267.e1-2267.e16. [Crossref] [PubMed]
- Westermark A, Hedén P, Aagaard E, et al. The use of TMJ Concepts prostheses to reconstruct patients with major temporomandibular joint and mandibular defects. Int J Oral Maxillofac Surg 2011;40:487-96. [Crossref] [PubMed]
- Aagaard E, Thygesen T. A prospective, single-centre study on patient outcomes following temporomandibular joint replacement using a custom-made Biomet TMJ prosthesis. Int J Oral Maxillofac Surg 2014;43:1229-35. [Crossref] [PubMed]
- Mommaerts MY, Nicolescu I, Dorobantu M, et al. Extended Total Temporomandibular Joint Replacement with Occlusal Adjustments: Pitfalls, Patient-reported Outcomes, Subclassification, and a New Paradigm. Ann Maxillofac Surg 2020;10:73-9. [Crossref] [PubMed]
- Saeed N, Hensher R, McLeod N, et al. Reconstruction of the temporomandibular joint autogenous compared with alloplastic. Br J Oral Maxillofac Surg 2002;40:296-9. [Crossref] [PubMed]
- Gerbino G, Zavattero E, Berrone S, et al. One stage treatment of temporomandibular joint complete bony ankylosis using total joint replacement. J Craniomaxillofac Surg 2016;44:487-92. [Crossref] [PubMed]
- De Meurechy N, Mommaerts MY. Alloplastic temporomandibular joint replacement systems: a systematic review of their history. Int J Oral Maxillofac Surg 2018;47:743-54. [Crossref] [PubMed]
- Amarista FJ, Mercuri LG, Perez D. Temporomandibular Joint Prosthesis Revision and/or Replacement Survey and Review of the Literature. J Oral Maxillofac Surg 2020;78:1692-703. [Crossref] [PubMed]
- Mercuri LG. Alloplastic temporomandibular joint replacement: rationale for the use of custom devices. Int J Oral Maxillofac Surg 2012;41:1033-40. [Crossref] [PubMed]
Cite this article as: Borbon C, Zavattero E, Ramieri G, Gerbino G. Management of failed autogenous tissues temporomandibular joint reconstruction: case series and literature review. Front Oral Maxillofac Med 2023;5:40.

