Virtual surgical planning in fibula flap mandibular reconstruction
Introduction
Head and neck microsurgical reconstruction has evolved in the last two decades with the development and popularization of virtual surgical planning (VSP) and computer-aided design and manufacturing (CAD-CAM). Optimal mandibular reconstruction following oncological resections requires microvascular free flaps such as fibula or iliac crest. Fibula-free flap is nowadays considered the gold standard for mandibular reconstruction (1). Its abundance of bone stock, pedicle length and minor donor-site morbidity make it suitable due to its versatility and reliability (2,3).
When reconstructing a mandible due to oncological or traumatic defect, the traditional free-hand technique requires high-precision skill for hand-crafting the bony flap to for adequate adaptation to the defect. This can be time-consuming in complex defects that require multiple osteotomies to fully restore the curvature of the mandible and can also frequently lead to imperfect outcomes at both functional and aesthetical levels (4-6).
Application of VSP and CAD-CAM to bone free flaps has improved the precision of oncological margins and better flap segmentation and modelling. As a consequence, operating time is reduced and better aesthetic results are achieved.
In our unit, VSP and CAD-CAM is applied to every bone graft requiring complex segmentation and modelling. The objective of this article is to present our methodology, and describe the recommendations and disadvantages that have found from our experience.
Methodology: step-by-step
Although the utilization of VSP and CAD-CAM can differ between centers, the following steps are commonly used. Slight differences in application of the technology may be found between institutions. Since the fibula flap is the most widely used in mandibular reconstruction, we have chosen this as the model for the present article. Nonetheless, the principles and steps for execution are readily applicable to other bony microvascular free flaps such as iliac crest or scapula.
First, if a free fibula flap is chosen for a mandibular reconstruction, a high-resolution Angio-CT (1-mm cuts) of the facial skeleton and lower extremities should be obtained. Images should be obtained no more than 3 weeks before the surgery (2 weeks is considered optimal) in order to enhance the accuracy of oncological margins and prevent potential extirpative errors. Images of lower extremities should confirm the permeability of the three vascular axes of the legs. All the imaging tests are sent to the modelling company designated to create the VSP.
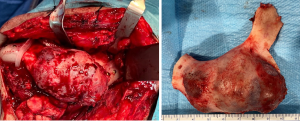
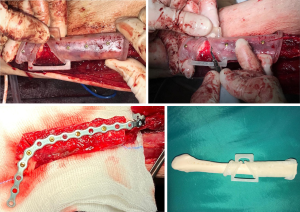
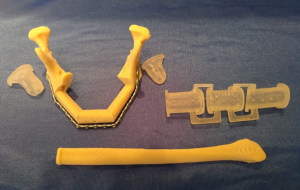
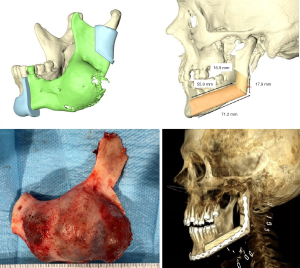
A web conference is then scheduled approximately 2 weeks before the surgery. A biomedical engineer from the company, the reconstructive surgeon and extirpative surgeons are always present to discuss each case. First, virtual resection of the tumor is conducted according to the indications of the extirpative surgeons. If desired, mandibular cut-guides are designed. Once the mandibular defect has been virtually created, reconstructive surgery recreates the new mandible with the fibula. Some important decisions should be made at this point: (I) laterality of donor fibula and orientation of the flap to prevent pedicle malposition; (II) osteotomies needed to recreate the mandible contour and osteosynthesis needed to secure the flap (miniplates vs. single plate; (III) location for placement of endosseous implants if previously decided. Whilst in the traditional technique, all these decisions were made by eye during surgery, the most notable difference with VSP is the possibility of producing a tridimensional design of the fibula osteotomies, which allows for finally recreating the native mandibular shape with greater accuracy. Based on the decisions described, a cutting guide for the fibula can then be designed, and the osteosynthesis plate or miniplates can be virtually modelled (Figures 1,2).
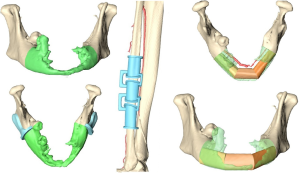
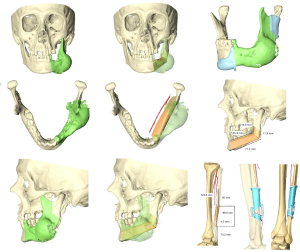
The next phase involves the creation of 3D models. It usually takes the modelling company between 7 and 10 days to deliver these to the hospital. When dealing with complex reconstructions (large resection of anterior mandible, delayed reconstruction after radiotherapy, etc.) we usually order stereolithographic models, mandibular cut guides to assure accuracy during ablative surgery, and fibula cutting guides and a pre-bent reconstruction plate to reduce modelling time and improve aesthetic outcomes. In less complex cases, only stereolithographic models and mandibular cutting guides are ordered. Fibula osteotomies are more intuitive and plate modelling is easily hand-bent over the stereolithographic model (Figure 3).
Surgery is carried out in a single step by two surgical teams. Mandibular resection is guided by predesigned cut splints attached to the mandible by a unicortical screw. Fibula flap harvest is made following the traditional technique except that that fibula cutting guides are fixed with a unicortical screw and osteotomies are carefully made with piezosurgery before clamping the pedicle. Thus, flap ischemia time is considerably reduced in comparison with the traditional hand-modelling technique.
Pitfalls
- When VSP is carried out with imaging tests obtained more than 3 weeks before the surgery, there is a high risk of making an error when designing the surgical margins. This could be rectified during the surgery by discarding all the virtual reconstruction planning. Otherwise, inadequate surgical margins would be obtained, thereby compromising oncological outcomes.
- Meticulous evaluation of lower-limb CT angiography should be carried out before VSP web conference. We recommend checking the permeability of the three vascular axes of the leg. Vascular abnormalities presence such as peroneal arteria magna may preclude the use of that side fibula due to the high risk of lower-limb ischemia
- Positioning of the cutting guides is critical during surgery. A perfect fit is essential in order to ensure that the virtual plan translates to the surgical setting. Bone exposure some centimeters beyond the location of the osteotomies is needed to effortlessly place and fix the guides. Fixation with unicortical screws allows for the subsequent use of the same holes for definitive plate fixation with bicortical screws (Figure 4).
- Due to the weakness of the acrylic material used for the cutting guides, manipulation should always be performed with extreme care. All surgery team members, including nurses, should be instructed in advance. Fracture of these pieces could result in the miss-adaptation of the guides and a loss of cut accuracy (Figure 5).
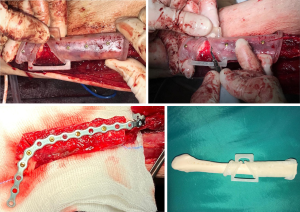 Figure 5 Case 2. Intraoperative photographs of the fibula free flap harvest. Excessive pressure screwing the cut guide produced a fracture of the proximal segment. Piezosurgery is a useful tool to prevent damage to the pedicle during osteotomies. Modelling and fixation of the fibula segments is performed before clamping the pedicle.
Figure 5 Case 2. Intraoperative photographs of the fibula free flap harvest. Excessive pressure screwing the cut guide produced a fracture of the proximal segment. Piezosurgery is a useful tool to prevent damage to the pedicle during osteotomies. Modelling and fixation of the fibula segments is performed before clamping the pedicle. - Cutting guide slots are usually wider than the saw. Unnoticed erroneous angulations of the cuts are allowed. When multiple cuts are required, accumulation of minor angulation mistakes can lead to the mismatch of bone fragments during osteosynthesis. In our experience, asking the VPS/CAD-CAM company for narrower cut-guide slots, in addition to using piezosurgery, can help to achieve more accurate cuts (Figure 5).
- Although not mandatory, in virtual planned cases some reconstructive microsurgeons prefer to perform osteotomies and osteosynthesis prior to clamping the pedicle and extracting the flap. Extreme care should be taken during saw manipulation and flap modelling to prevent damage to the pedicle. To the best or our knowledge piezosurgery osteotomies are more precise and safer, minimizing ischemia time without the risk of pedicle injuries (Figure 5).
Advantages
- Cleaner surgical margins;
- Decrease in ischemia and total operative time;
- More aesthetic and functional outcomes.
Disadvantages
- Increased presurgical (virtual planning) time;
- Increased economic costs;
- No improvement in postoperative complication rates.
Discussion
Free bone-flap conformation with respect to native mandibular contour is one of the most challenging issues in mandibular reconstruction. The introduction and subsequent popularization of 3D VSP has responded to the need for reconstructive surgeons to have a tool for improving the functional and aesthetic outcomes of their patients (Figure 6). Reconstructive accuracy is probably the most controversial outcome. Most reconstructive surgeons agree on the benefits offered by VSP and CAD-CAM when it comes to accomplishing high-precision reconstructions, particularly in cases of high complexity that require two or more osteotomy segments. In this regard, there are a number of studies that report statistical evidence. Several methods have been used to evaluate the accuracy of reconstruction, including condyle and gonial shift, differences between intergonial and gonial angles, or condyle-gonion and gonion-gnathion distances. These parameters of the remaining mandible and fibula segments have been compared pre- and postoperatively with an optimal outcome defined as either the virtual planned ideal outcome or a mirrored contralateral side. Even though authors such as Hanasono et al., Bouchet et al., Weitz et al. or De Maesschalck et al. have demonstrated a significant increase in accuracy when using CAD-CAM mandibular reconstruction compared with free hand mandibular reconstruction, the absence of a standardized procedure for assessing the accuracy of the methodology (anatomical landmark, time of postoperative CT scan, etc.) impedes the ability to obtain homogenous statistical significance (7-10). Authors such as Chang et al., however, argue that optimal accuracy outcomes can be achieved without VSP (11). To the best of our knowledge, the skills of an experienced surgeon make VSP unnecessary in cases of low-complexity reconstruction that require only one osteotomy.
One of the most widely studied issues in VSP is undoubtedly the reduction in ischemia and operative time. Simplification of bone graft cutting, molding, setting and fixation all have a direct impact on reconstructive surgery time (8,12-14). Moreover, the possibility of shaping the fibula before dividing the pedicle also minimizes ischemia time (8,12-16). Since reconstructive surgery time is reduced with VSP, this also shortens total operative time. Unfortunately, there are no studies that provide strong statistical evidence regarding the impact of VSP on postoperative clinical outcomes, including length of hospital stay.
Reconstructive microsurgeons are always concerned about major postoperative complications such as flap loss, fistula, or infection (9,13,17,18). Postoperative complication rates in VSP mandibular reconstructions have been reported in several studies. Whilst some studies have observed lower complication rates in computer-assisted reconstructions, two meta-analyses conducted by Powcharoen et al. and Tang et al. found no statistically significant differences in these outcomes when comparing VSP free flap reconstructions with conventional procedures (19-22).
High cost is the main disadvantage of using VSP and CAD-CAM technology. To the best or our knowledge, only two studies have investigated the economic viability of computer-assisted reconstructions (19,23). Although this technology can be more cost-effective when using freely available open source software, a specialized medical company is usually contracted for this purpose. In the US, the direct costs of each VSP and CAD-CAM mandibular reconstruction vary between $3,000 and $12,000 per case depending on the company and hardware ordered (7,24). There are currently no clear estimates of the economic savings derived from reducing total operative time when using this technology. In the US, the cost per minute of each operating room is estimated to be between $50 and $100 (25). Therefore, any increase in efficiency could potentially offset the costs of this technology. However, health insurance coverage and costs related to operative time vary between countries and health centers. Furthermore, VSP ablative surgery could reduce the need for medium and long-term oncological treatments, although further research is needed in this field. It is expected that the current popularity of CAD-CAM software will increase the competition among VSP companies in the future, and thus drive down the costs of this technology.
Conclusions
The VSP and CAD-CAM technology is here to stay. The accuracy assured by this technology when performing complex reconstructions, and the efficiency in reducing ischemic time, reconstructive time, and total operative time make of this technology a powerful tool that can be used by experienced reconstructive microsurgeons. The high costs incurred can be outweighed by the economic savings resulting from a reduction in operative time. Prospective, randomized controlled trials are required to definitively assess the accuracy of this technology in comparison with free-hand reconstructions and establish the basis of indication protocols for computer-assisted reconstruction. Our recommendation is to use a case-by-case evaluation to select those patients for whom VSP will help to obtain the best aesthetical and functional outcomes.
Acknowledgments
The authors would like to acknowledge Eric Wizauer for critical assistance with image procurement and figure development.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Paolo Cariati) for the series “Microvascular reconstruction of head and neck oncological defects—state of the art” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.org/article/view/10.21037/fomm-2020-mr-03/coif). The series “Microvascular reconstruction of head and neck oncological defects—state of the art” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hidalgo DA, Rekow A. A review of 60 consecutive fibula free flap mandible reconstructions. Plast Reconstr Surg 1995;96:585-96; discussion 597-602. [Crossref] [PubMed]
- Wei FC, Santamaria E, Chang YM, et al. Mandibular reconstruction with fibular osteoseptocutaneous free flap and simultaneous placement of osseointegrated dental implants. J Craniofac Surg 1997;8:512-21. [Crossref] [PubMed]
- Ferri J, Piot B, Ruhin B, et al. Advantages and limitations of the fibula free flap in mandibular reconstruction. J Oral Maxillofac Surg 1997;55:440-8; discussion 448-9. [Crossref] [PubMed]
- Leiggener CS, Krol Z, Gawelin P, et al. A computer-based comparative quantitative analysis of surgical outcome of mandibular reconstructions with free fibula microvascular flaps. J Plast Surg Hand Surg 2015;49:95-101. [Crossref] [PubMed]
- Brown JS, Shaw RJ. Reconstruction of the maxilla and midface: introducing a new classification. Lancet Oncol 2010;11:1001-8. [Crossref] [PubMed]
- Wijbenga JG, Schepers RH, Werker PMN, et al. A systematic review of functional outcome and quality of life following reconstruction of maxillofacial defects using vascularized free fibula flaps and dental rehabilitation reveals poor data quality. J Plast Reconstr Aesthet Surg 2016;69:1024-36. [Crossref] [PubMed]
- Hanasono MM, Skoracki RJ. Computer-assisted design and rapid prototype modeling in microvascular mandible reconstruction. Laryngoscope 2013;123:597-604. [Crossref] [PubMed]
- Bouchet B, Raoul G, Julieron B, et al. Functional and morphologic outcomes of CAD/CAM-assisted versus conventional microvascular fibular free flap reconstruction of the mandible: A retrospective study of 25 cases. J Stomatol oral Maxillofac Surg 2018;119:455-60. [Crossref] [PubMed]
- Weitz J, Bauer FJM, Hapfelmeier A, et al. Accuracy of mandibular reconstruction by three-dimensional guided vascularised fibular free flap after segmental mandibulectomy. Br J Oral Maxillofac Surg 2016;54:506-10. [Crossref] [PubMed]
- De Maesschalck T, Courvoisier DS, Scolozzi P. Computer-assisted versus traditional freehand technique in fibular free flap mandibular reconstruction: a morphological comparative study. Eur Arch Otorhinolaryngol 2017;274:517-26. [Crossref] [PubMed]
- Chang EI. My first 100 consecutive microvascular free flaps: pearls and lessons learned in first year of practice. Plast Reconstr Surg Glob Open 2013;1:e27 [Crossref] [PubMed]
- Seruya M, Fisher M, Rodriguez ED. Computer-assisted versus conventional free fibula flap technique for craniofacial reconstruction: an outcomes comparison. Plast Reconstr Surg 2013;132:1219-28. [Crossref] [PubMed]
- Bao T, He J, Yu C, et al. Utilization of a pre-bent plate-positioning surgical guide system in precise mandibular reconstruction with a free fibula flap. Oral Oncol 2017;75:133-9. [Crossref] [PubMed]
- Culié D, Dassonville O, Poissonnet G, et al. Virtual planning and guided surgery in fibular free-flap mandibular reconstruction: A 29-case series. Eur Ann Otorhinolaryngol Head Neck Dis 2016;133:175-8. [Crossref] [PubMed]
- Ayoub N, Ghassemi A, Rana M, et al. Evaluation of computer-assisted mandibular reconstruction with vascularized iliac crest bone graft compared to conventional surgery: a randomized prospective clinical trial. Trials 2014;15:114. [Crossref] [PubMed]
- Rustemeyer J, Sari-Rieger A, Melenberg A, et al. Comparison of intraoperative time measurements between osseous reconstructions with free fibula flaps applying computer-aided designed/computer-aided manufactured and conventional techniques. Oral Maxillofac Surg 2015;19:293-300. [Crossref] [PubMed]
- Ciocca L, Marchetti C, Mazzoni S, et al. Accuracy of fibular sectioning and insertion into a rapid-prototyped bone plate, for mandibular reconstruction using CAD-CAM technology. J Craniomaxillofac Surg 2015;43:28-33. [Crossref] [PubMed]
- Zhang L, Liu Z, Li B, et al. Evaluation of computer-assisted mandibular reconstruction with vascularized fibular flap compared to conventional surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 2016;121:139-48. [Crossref] [PubMed]
- Tarsitano A, Battaglia S, Crimi S, et al. Is a computer-assisted design and computer-assisted manufacturing method for mandibular reconstruction economically viable? J Craniomaxillofac Surg 2016;44:795-9. [Crossref] [PubMed]
- Ritschl LM, Mücke T, Fichter A, et al. Functional Outcome of CAD/CAM-Assisted versus Conventional Microvascular, Fibular Free Flap Reconstruction of the Mandible: A Retrospective Study of 30 Cases. J Reconstr Microsurg 2017;33:281-91. [Crossref] [PubMed]
- Powcharoen W, Yang WF, Yan Li K, et al. Computer-Assisted versus Conventional Freehand Mandibular Reconstruction with Fibula Free Flap: A Systematic Review and Meta-Analysis. Plast Reconstr Surg 2019;144:1417-28. [Crossref] [PubMed]
- Tang NSJ, Ahmadi I, Ramakrishnan A. Virtual surgical planning in fibula free flap head and neck reconstruction: A systematic review and meta-analysis. J Plast Reconstr Aesthet Surg 2019;72:1465-77. [Crossref] [PubMed]
- Zweifel DF, Simon C, Hoarau R, et al. Are virtual planning and guided surgery for head and neck reconstruction economically viable? J Oral Maxillofac Surg 2015;73:170-5. [Crossref] [PubMed]
- Toto JM, Chang EI, Agag R, et al. Improved operative efficiency of free fibula flap mandible reconstruction with patient-specific, computer-guided preoperative planning. Head Neck 2015;37:1660-4. [Crossref] [PubMed]
- Macario A. What does one minute of operating room time cost? J Clin Anesth 2010;22:233-6. [Crossref] [PubMed]
Cite this article as: Monsalve-Iglesias F, Martinez-Sahuquillo Rico Á, Fraile-Ruiz L. Virtual surgical planning in fibula flap mandibular reconstruction. Front Oral Maxillofac Med 2020;2:12.