
Indications for alloplastic temporomandibular joint replacement in maxillofacial surgery for benign lesions: a review of the literature and clinical cases
Introduction
Thanks to the contemporary genetic and molecular biology diagnostic options now available, huge progress has been made with classifying tumors in the temporomandibular joint (TMJ) area. The main reference to tumor biology, prognostication, classification, and treatment is still the 2020 5th Edition of the World Health Organization (WHO) classification of tumors, including benign lesions of the TMJ (1). The goal of this paper is not to give a histopathological update on benign lesions of the TMJ. Nevertheless, some aspects of the reclassification in 2020 compared to the 2013 WHO classification are mentioned. The aneurysmal bone cyst is reclassified as an osteoclastic giant cell-rich tumor, and the simple bone cyst as another mesenchymal tumor of bone in the same group as Adamantinoma and fibrous dysplasia. Concerning the biological potential, the chondroblastoma changed from intermediate (rarely metastasizing) to benign tumor, the synovial chondromatosis from a benign tumor to intermediate (locally aggressive) and the aneurysmal bone cyst from intermediate (locally aggressive) to a benign tumor (2).
All anatomic parts of the TMJ have the potential to be the origin of a neoplastic disease—the temporal and mandibular condylar bone and overlying fibrocartilage, synovial lining, articular disk, fibrous capsule, and ligaments. The following clinical symptoms should elicit concern for a benign neoplastic disease of the TMJ area: pain in the TMJ area, limited mandibular range of motion, deviation of the mandible during the opening, joint sounds (e.g., crepitation), swelling around the TMJ area, progressive open bite on the affected side, crossbite on the non-affected side, the progressive facial asymmetry with a deviation of the chin to the non-affected side, pathological fractures, otologic complaints, increased severity of symptoms, and atypical response to any conservative treatment.
In a review of the clinical and radiological signs of TMJ pseudotumors and 19 tumors, Poveda-Roda et al. (2) summarized which signs distinguished them from true benign and malignant neoplasia. These authors found the most frequent lesions were pseudotumors (synovial chondromatosis, pigmented villonodular synovitis, eosinophilic granuloma and osteochondroma). Approximately 20% of these pseudotumors had been initially misdiagnosed and treated as TMJ dysfunction (TMD), with pain, swelling, and limitation of joint movements being the most frequent clinical signs. The authors point out that panoramic imaging alterations were not observed in 14.6% of the benign tumors and 7.7% of the malignant lesions. This emphasizes the need for the clinician to be alert to these diseases while also raising the question of the need for additional (three-dimensional) radiological imaging.
In summary, the main challenge for a clinician treating TMJ patients is understanding the complexity of diagnosing and managing the “typical” TMD patient with functional TMJ disorders. This enables the clinician to be familiar with these patients’ typical clinical course and be alert to the potential of neoplastic or other pathological conditions in the TMJ area.
When it comes to the management options available for benign TMJ lesions, questions have been raised about how aggressive treatment should be (e.g., in case of synovial chondromatosis) and possible joint reconstruction techniques (e.g., autologous vs. alloplastic reconstruction).
This paper will aim to present a narrative review of the English language surgical literature relative to the indications for the use of TMJ replacement (TMJR) devices in the management of the reconstruction of benign mandibular lesions either involving the TMJ primarily or secondarily and to present examples of different clinical situations after alloplastic TMJR in the long term follow up. We present this article in accordance with the Narrative Review reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-41/rc).
Methods
A narrative literature review was performed using the relevant database PubMed. An electronic search was complemented by an iterative hand search in the reference lists of the already identified articles. The endpoint of the literature search was August 12, 2022. Endnote 20 was used for the electronic management of the literature (search strategy summary in Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of Search | August 12, 2022 |
| Databases and other sources searched | PubMed |
| Search terms used | ((temporomandibular joint replacement) OR (total temporomandibular joint replacement) OR (temporomandibular endoprosthesis) OR (alloplastic temporomandibular reconstruction)) AND ((benign tumor) OR (benign lesion) OR (benign neoplasia) OR (odontogenic tumor)) |
| Timeframe | All till August 12, 2022 |
| Inclusion and exclusion criteria | Inclusion criteria: publications in English, clinical studies including retrospective and prospective clinical trials, observational studies, cross-sectional studies, cohort studies, case series and case reports. Exclusion criteria: autogenous reconstruction, alloplastic reconstruction without fossa component, underlying malignant disease, degenerative disease inclusive ankylosis |
| Selection process | The selection process was conducted by the author HN; in case of a questionable decision, a consensus together with MT was gained |
The identified studies were screened based on the title and keywords, followed by an assessment based on the abstracts and followed by an assessment based on the full text. Before the literature review, the following criteria for literature evaluation were defined. The inclusion criteria were: publications in English, clinical studies including retrospective and prospective clinical trials, observational studies, cross-sectional studies, cohort studies, case series and case reports. The exclusion criteria were: autogenous reconstruction, alloplastic reconstruction without fossa component, underlying malignant disease, and degenerative disease, including ankylosis.
Main body
The electronic search found a total of 137 potentially relevant titles. One-hundred-one publications were excluded from the first screening based on the title and keywords. Additionally, 18 titles were excluded based on the abstract evaluation. Eighteen full-text articles were thoroughly evaluated. Four papers had to be excluded at this stage because they did not fulfill the inclusion criteria of the present review. Fourteen articles could be included (3-16) (Figure 1). The literature included nine case reports, four case series and one retrospective trial (Table 2).
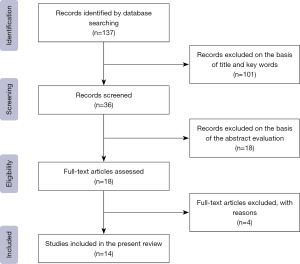
Table 2
| Year of publication | Authors | Study design | Underlying diagnosis | Count of patients | Type of TMJR | Timepoint of reconstruction | Origin of reconstruction |
|---|---|---|---|---|---|---|---|
| 2022 | Horen et al. (3) | Case report & review | Ameloblastoma | 1 | Custom | Immediate | Alloplastic |
| 2021 | Hurrell et al. (4) | Case report | Osteochondroma | 1 | Custom | Immediate | Alloplastic + osteotomy contralateral |
| 2020 | Blackhall et al. (5) | Case report and literature review | Arteriovenous malformation | 1 | Custom | Immediate | Alloplastic |
| 2019 | Zheng et al. (6) | Case series | Giant cell lesion and osteochondroma | 5 | Custom | Immediate | Alloplastic (scull base-TMJ) |
| 2018 | Sarlabous et al. (7) | Case series | Ameloblastoma and recurrence | 3 | Custom | Immediate | Alloplastic + iliac crest |
| 2018 | Xu et al. (8) | Case series | Giant condylar osteoma | 3 | Stock | Immediate | Alloplastic |
| 2017 | de Souza et al. (9) | Case report | Osteoma | 1 | Custom | Immediate | Alloplastic |
| 2016 | Mehra et al. (10) | Retrospective study | Osteochondroma | 11 | Custom | Immediate | Alloplastic |
| 2014 | Morrison et al. (11) | Case report | Recurrence of ameloblastoma | 1 | Custom | Immediate | Alloplastic + iliac crest |
| 2014 | Ruiz Valero et al. (12) | Case series | Ameloblastoma | 2 | Custom | Immediate | Alloplastic |
| 2013 | Zavattero et al. (13) | Case report | Ossifying fibroma | 1 | Stock | Immediate | Alloplastic |
| 2012 | Ramos-Murguialday et al. (14) | Case report | Osteochondroma | 1 | Stock | Immediate | Alloplastic |
| 2011 | Morey-Mas et al. (15) | Case report | Osteochondroma | 1 | Stock | Immediate | Alloplastic |
| 1996 | Karras et al. (16) | Case report | Osteochondroma | 1 | Custom | Immediate | Alloplastic |
TMJR, temporomandibular joint replacement; TMJ, temporomandibular joint.
The underlying diagnoses for total TMJR were: ameloblastoma, osteochondroma, arteriovenous malformation, giant cell lesion, giant osteoma, osteoma, ossifying fibroma, and recurrences of ameloblastoma. Before 2013, the included literature mainly reports on cases using stock endoprostheses. In the more recent literature, there seems to be a tendency towards custom-made endoprostheses. In all reported cases of benign lesions, an immediate alloplastic reconstruction of the TMJ could be achieved. In most cases, pure alloplastic reconstruction of the TMJ was performed, and only one case report and a series of three cases report on a combined reconstruction using a custom endoprosthesis and an autogenous iliac crest graft for the treatment of recurrent ameloblastoma (7,11). In one case of the treatment of an osteochondroma, the alloplastic reconstruction was combined with a contralateral sagittal split to correct the condylar position (4). One case series reports about five cases of large and extensive lesions that involve scull base destruction and result in extensive resections demanding for a combined scull base-TMJ prosthesis (6).
Classification based on time of reconstruction
When a TMJR prosthesis is being considered for the reconstruction of a mandibular defect created by the removal of a benign lesion involving the TMJ, cases can be classified based on the time in which the reconstruction is going to be performed: immediate primary TMJ reconstruction; delayed primary TMJ reconstruction; and delayed secondary TMJ reconstruction
This classification is useful in different clinical scenarios and pathologies, here adopted for benign TMJ lesions. There are unique concerns associated with the reconstruction of mandibular segmental defects, including the TMJ created after removing a benign lesion. The nature of the lesion may require removal not only of the involved mandibular lesion and bone but also any associated affected intraoral soft tissues and teeth. This results in significant functional, esthetic, and occlusal consequences, as well as consideration of the oral flora’s contamination of the surgical site. Patient evaluation and management planning for these cases vary depending on the specific clinical presentation and the sequence of the reconstruction:
Immediate primary TMJ reconstruction
Immediate primary reconstruction with a TMJR prosthesis can be accomplished in one stage and utilized in patients that require a mandibular resection involving the TMJ to address the removal of the pathology. This approach is indicated in “truly” benign diseases where the risk of a positive margin is the lowest.
Once the pathological diagnosis has been confirmed, the surgeon must decide on the extent of the mandibular resection and if immediate reconstruction is possible. The extent of the resection will dictate whether a stock or custom TMJR device, either standard or eTMJR, will be used. Stock TMJR devices can only be utilized in cases with sufficient inferior ramus left into which an adequate number of fixation screws can be placed to ensure the functional stability of the device components.
In most cases, due to the amount of mandible that must be resected to include good tumor margins, a custom TMJR is chosen. A specific protocol computer tomography (CT) scan is made from which a stereolithographic (SL) model is developed, upon which the final TMJR device is designed and manufactured.
The resection is carried out utilizing virtual surgical planning (VSP), the device is designed for the specific case, and the TMJR is manufactured. Cutting guides are developed for use at the surgery to guide the resection and proper placement of the TMJR components. Cases of primary TMJ reconstruction with concomitant mandibular bone grafting with iliac crest bone grafting have been described in the literature (11,12,17,18).
Delayed primary TMJ reconstruction
Delayed primary TMJ reconstruction is indicated for patients who previously had undergone primary pathology surgery where immediate reconstruction was contraindicated, such as large lesions requiring both intraoral and extraoral exposure for removal, or where local significant oral soft tissue required removal with the lesion requiring placement of a vascularized flap. Both of these scenarios have the increased potential for developing a post-reconstruction infection. Also, other infections or medical conditions of the patient might be reasons for delayed reconstruction. Only a custom TMJR device can be considered for such cases. This approach is indicated in locally aggressive benign diseases where complete removal needs to be ensured, and a delay of resections needs to be avoided.
Preoperative evaluation and surgical planning of delayed primary TMJ reconstruction involve a review of the prior surgery to understand the nature of the deformity. The same presurgical CT and VSP protocol can be followed for immediate primary reconstruction cases. In most cases, malocclusion exists as the mandible shifts to the affected side. This requires the fabrication of a two-piece SL model. Using VSP, surgeons and design engineers establish the proper occlusion and the final surgical splint. The utilization of custom 3D antibiotic-impregnated polymethylmethacrylate (PMMA) spacers in these delayed primary TMJ reconstruction cases has been described in the literature (19,20).
Delayed secondary TMJ reconstruction
Delayed secondary TMJ reconstruction is performed for the multiple-operated patient who has undergone failed or failing previous autogenous or alloplastic reconstructions, often in combination with insufficient soft tissue support. Therefore, when evaluating these patients, the surgeon must determine the reasons for the poor outcome so as not to repeat them or use the same device.
Only custom TMJR devices should be considered for the management of these cases. Any failed or failing devices present must be removed before the protocol CT scan to avoid artifacts. At the device removal surgery, the surgeon must reestablish the correct maxillomandibular relationship by using a silicon or an antibiotic-impregnated PMMA spacer if an infection is associated with the prior device failure (20,21). This enables a later reconstruction by keeping the periosteal tube open to preserve the facial nerve and acts bactericidal. Although in easier cases, an antibiotic-impregnated spacer is not mandatory.
Presentation of clinical cases
The complexities involved in managing the reconstruction of these cases present a unique surgical challenge to the surgeon. The extent of the lesion and resultant reconstruction may require larger or modified surgical access, while others may require identification and preservation of the inferior alveolar neurovascular bundle or possibly a combined bone graft. However, the basic surgical principles for the implantation of TMJR devices apply.
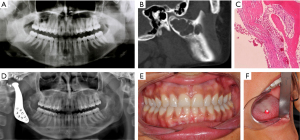
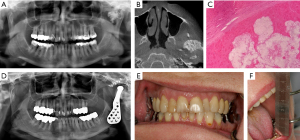
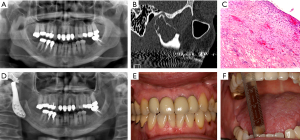
The following cases illustrate the value of TMJ reconstruction after ablative surgery for benign lesions in the mandible (Table 3, Figure 2-4).
Table 3
| Characteristic | Case 1 | Case 2 | Case 3 |
|---|---|---|---|
| Gender/age (years) | Female/22 | Female/51 | Female/51 |
| Diagnosis | Aneurysmatic bone cyst, right TMJ | Pseudogout, left TMJ | Odontogenic myxoma, right TMJ |
| History | Progressive pain, limited mouth opening and swelling preauricular right | Progressive swelling preauricular left and restrictions of mouth opening | No functional or esthetic complaints, secondary finding via dental X-ray examination |
| Histology | HE staining, 10×: cyst wall covered by a thin, flat cell layer and small clots of blood (left side), transition to the bone in the right half | HE staining, 10×: cartilaginous tissue in the center and lower half with embedded cloud-like bright spaces, consistent with dissolved crystal depositions, covered by fibrous connective tissue | HE staining, 10×: fiber-rich wall with cyst-like configuration, smooth surface, tissue focally with a myxoid configuration (upper half of the picture in the subsurface area with associated hemorrhage) |
| System/custom or stock | Biomet-Zimmer/custom | Biomet-Zimmer/stock | TMJ Concepts-Stryker/custom |
| Follow-up (years) | 8 | 7 | 8 |
| Mouth opening capacity (mm) | 45 | 50 | 34 |
| VAS (0: indicates no pain, no diet restrictions, normal jaw function, no disability; 10: indicates worst pain imaginable, liquids only, no jaw movements, totally disability) | VAS pain 2/10 | VAS pain 0/10 | VAS pain 0/10 |
| VAS dietary restrictions 0/10 | VAS dietary restrictions 0/10 | VAS dietary restrictions 0/10 | |
| VAS jaw movement 2/10 | VAS jaw movement 4/10 | VAS jaw movement 2/10 | |
| VAS disability 0/10 | VAS disability 0/10 | VAS disability 0/10 |
TMJ, temporomandibular joint; HE, hematoxylin eosin; VAS, Visual Analogue Scale.
Discussion
Successful outcomes in managing the end-stage joint disease with alloplastic joint replacement devices in orthopedic and maxillofacial surgery have been well-documented for decades (17,18,22-24). However, evidence for using TMJR to reconstruct mandibular defects created by removing benign mandibular lesions has been sparse.
The primary goals of mandibular reconstruction involving the TMJ after benign disease ablative surgery are a return to normal mandibular function and form by restoring continuity and developing a stable base upon which a functional dental occlusion can be established.
Several surgical options have been proposed to achieve these goals utilizing either autogenous tissues or alloplastic devices. The indications for each are contingent on the size of the defect, the patient’s age and medical history, their willingness to cooperate with post-reconstruction physical therapy, and, most frequently, the surgeon’s preference and experience with each procedure (21).
Patient selection is important to the long-term outcomes of each of these mandibular reconstruction options. This paper presented some general indications for the reconstruction of mandibular defects involving the TMJ based on a time-of-reconstruction-related classification scheme.
The classification schemes and management algorithms presented are meant to assist in the reconstruction option decision-making process. Although some protocols exist for managing mandibular defects, few describe the reconstruction of acquired mandibular defects involving the TMJ. Potter and Dierks proposed a classification of mandibular defects involving the TMJ where distinctions are made based on the lesion and size of the resultant defect, disk salvageable or not, and fossa salvageable or not. These authors focus only on autogenous reconstruction (25). Bredell et al. proposed similar recommendations, the difference being that the latter’s algorithm was developed considering the anatomical structures to be salvaged at the ablation surgery and for complication risk factors (26). The authors also mention alloplastic TMJR as a therapeutic option.
Large mandibular defect reconstruction with TMJR devices has been reported, mainly small case series or single case reports (11,12,17,18,27,28). Therefore, the lack of strong evidence-based literature for using TMJR devices in these cases makes developing definitive management algorithms difficult. Therefore, to date, individual management decisions have depended on the surgeon’s experiences using TMJR devices.
Presently, stock and custom or patient-fitted TMJR devices are available. Usage of stock TMJR devices is limited to mandibular defects involving the condyle and the superior mandibular ramus. However, a case of combined microvascular free bone transfers and a stock TMJR device has been reported (20). Since custom TMJR devices are made to fit each case, they can closely mimic the missing local TMJ anatomy. Further, custom extended devices (eTMJR) allow for the replacement of large and complex mandibular defects (21). Elledge et al. have proposed an eTMJR classification system (29) which has been validated (30).
As a downside of eTMJR in tooth-bearing parts of the mandible, these types of reconstruction compromise the option of placing dental implants in vascularized bone without stress protection. Typically, eTMJR devices provide holes to fix bone (vascularized or not vascularized). An alternative is the combination of standard TMJR devices with, e.g., a bony fibula transplant (21).
Considering the small number of reports in the literature and the relatively small number of benign lesions managed using TMJ prostheses, the authors conclude that if the benign pathology involves the temporomandibular complex, an evidence-based conclusion about safety, success rate, and long-term stability is not possible. Based on recent literature, custom-made TMJ prostheses seem to be used more commonly because they are clinically very predictable and stable. In contrast, chondrocostal grafts (widely used in the past) are highly unpredictable in growing patients (31). Bredell et al. report the complication rate of different TMJ—subcomponent reconstruction techniques and point out the unpredictability of costochondral graft (26).
The patient-specific design of the components increases the precision of anatomical reconstruction and long-term stability. However, the indication for condylar resection in benign mandibular pathology is controversial. While some authors prefer incomplete condylectomy followed by orthognathic measures as the option of choice, others prefer complete condylectomy followed by TMJ reconstruction. Sometimes, the decision not to reconstruct the TMJ might be an option. Besides shifting the remnant mandible to the affected side with deviation while opening, sometimes with malocclusion, patients often do not complain a lot and develop a reasonably good function (23).
Nevertheless, alloplastic reconstruction using custom-made prostheses of the latest generation is a safe, reliable, and predictable therapeutic option (23). It expands the spectrum of reconstructive procedures and is an option to avoid donor side morbidity caused by autogenous grafts while achieving appropriate functional and aesthetic outcomes.
Conclusions
Based on the literature cited in this paper, TMJR devices are a reasonable approach to reconstructing benign mandibular lesions involving the TMJ, especially when a primary reconstruction is possible. More research must be done to prove the concept of alloplastic TMJR in cases when a delayed primary or secondary reconstruction is necessary.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Louis G. Mercuri) for the series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-41/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-41/coif). The series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- World Health Organization. Soft Tissue and Bone Tumours, 5th Edition, Volume 3. Lyon (France): International Agency for Research on Cancer, 2020.
- Poveda-Roda R, Bagán JV, Sanchis JM, et al. Pseudotumors and tumors of the temporomandibular joint. A review. Med Oral Patol Oral Cir Bucal 2013;18:e392-402. [Crossref] [PubMed]
- Horen SR, Hansdorfer MA, Seu M, et al. Alloplastic Temporomandibular Joint Reconstruction Following Recurrent Ameloblastoma Resection. J Craniofac Surg 2022;33:284-8. [Crossref] [PubMed]
- Hurrell M, Khabaz-Saberi S, Ricciardo PV. Management of deformity inducing osteochondroma of the temporomandibular joint: a case report. Aust Dent J 2021;66:337-9. [Crossref] [PubMed]
- Blackhall KK, Ling E, Kunjur J. A rare case of a intraosseous arteriovenous malformation of the temporomandibular joint and mandible - Case report and literature review. Int J Surg Case Rep 2020;76:394-8. [Crossref] [PubMed]
- Zheng JS, Liu XH, Chen XZ, et al. Customized skull base-temporomandibular joint combined prosthesis with 3D-printing fabrication for craniomaxillofacial reconstruction: a preliminary study. Int J Oral Maxillofac Surg 2019;48:1440-7. [Crossref] [PubMed]
- Sarlabous M, Psutka DJ. Treatment of Mandibular Ameloblastoma Involving the Mandibular Condyle: Resection and Concomitant Reconstruction With a Custom Hybrid Total Joint Prosthesis and Iliac Bone Graft. J Craniofac Surg 2018;29:e307-14. [Crossref] [PubMed]
- Xu X, Ma H, Jin S. One-Stage Treatment of Giant Condylar Osteoma: Alloplastic Total Temporomandibular Joint Replacement Aided by Digital Templates. J Craniofac Surg 2018;29:636-9. [Crossref] [PubMed]
- de Souza NT, Cavalcante RCL, de Albuquerque Cavalcante MA, et al. An unusual osteoma in the mandibular condyle and the successful replacement of the temporomandibular joint with a custom-made prosthesis: a case report. BMC Res Notes 2017;10:727. [Crossref] [PubMed]
- Mehra P, Arya V, Henry C. Temporomandibular Joint Condylar Osteochondroma: Complete Condylectomy and Joint Replacement Versus Low Condylectomy and Joint Preservation. J Oral Maxillofac Surg 2016;74:911-25. [Crossref] [PubMed]
- Morrison MD, Psutka DJ. Reconstruction of the temporomandibular joint after surgical ablation of a multiply recurrent ameloblastoma: a case report. J Can Dent Assoc 2014;80:e14. [PubMed]
- Ruiz Valero CA, Duran-Rodriguez G, Solano-Parra N, et al. Immediate total temporomandibular joint replacement with TMJ concepts prosthesis as an alternative for ameloblastoma cases. J Oral Maxillofac Surg 2014;72:646.e1-12. [Crossref] [PubMed]
- Zavattero E, Garzino-Demo P, Berrone S. Ossifying fibroma affecting the mandibular condyle: report of an uncommon case. J Craniofac Surg 2013;24:e351-3. [Crossref] [PubMed]
- Ramos-Murguialday M, Morey-Mas MÁ, Janeiro-Barrera S, et al. Osteochondroma of the temporomandibular joint: report of 2 cases emphasizing the importance of personalizing the surgical treatment. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;113:e41-7. [Crossref] [PubMed]
- Morey-Mas MA, Caubet-Biayna J, Iriarte-Ortabe JI. Osteochondroma of the temporomandibular joint treated by means of condylectomy and immediate reconstruction with a total stock prosthesis. J Oral Maxillofac Res 2011;1:e4. [PubMed]
- Karras SC, Wolford LM, Cottrell DA. Concurrent osteochondroma of the mandibular condyle and ipsilateral cranial base resulting in temperomandibular joint ankylosis: report of a case and review of the literature. J Oral Maxillofac Surg 1996;54:640-6. [Crossref] [PubMed]
- Rodrigues DB, Wolford LM, Malaquias P, et al. Concomitant treatment of mandibular ameloblastoma and bilateral temporomandibular joint osteoarthritis with bone graft and total joint prostheses. J Oral Maxillofac Surg 2015;73:63-74. [Crossref] [PubMed]
- Landes C, Korzinskas T, Dehner JF, et al. One-stage microvascular mandible reconstruction and alloplastic TMJ prosthesis. J Craniomaxillofac Surg 2014;42:28-34. [Crossref] [PubMed]
- Teschke M, Christensen A, Far F, et al. Digitally designed, personalized bone cement spacer for staged TMJ and mandibular reconstruction - Introduction of a new technique. J Craniomaxillofac Surg 2021;49:935-42. [Crossref] [PubMed]
- Green JM 3rd, Lawson ST, Liacouras PC, et al. Custom Anatomical 3D Spacer for Temporomandibular Joint Resection and Reconstruction. Craniomaxillofac Trauma Reconstr 2016;9:82-7. [Crossref] [PubMed]
- Vega LG, González-García R, Louis PJ. Reconstruction of acquired temporomandibular joint defects. Oral Maxillofac Surg Clin North Am 2013;25:251-69. [Crossref] [PubMed]
- Balel Y, Tümer MK. A Bibliometric Analysis of International Publication Trends in Total Temporomandibular Joint Replacement Research (1986-2020). J Oral Maxillofac Surg 2021;79:1458.e1-1458.e12. [Crossref] [PubMed]
- Wolford LM, Mercuri LG, Schneiderman ED, et al. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg 2015;73:952-60. [Crossref] [PubMed]
- Knight SR, Aujla R, Biswas SP. Total Hip Arthroplasty - over 100 years of operative history. Orthop Rev (Pavia) 2011;3:e16. [PubMed]
- Potter JK, Dierks EJ. Vascularized options for reconstruction of the mandibular condyle. Semin Plast Surg 2008;22:156-60. [Crossref] [PubMed]
- Bredell M, Grätz K, Obwegeser J, et al. Management of the temporomandibular joint after ablative surgery. Craniomaxillofac Trauma Reconstr 2014;7:271-9. [Crossref] [PubMed]
- Westermark A, Hedén P, Aagaard E, et al. The use of TMJ Concepts prostheses to reconstruct patients with major temporomandibular joint and mandibular defects. Int J Oral Maxillofac Surg 2011;40:487-96. [Crossref] [PubMed]
- Tang W, Long J, Feng F, et al. Condyle replacement after tumor resection: comparison of individual prefabricated titanium implants and costochondral grafts. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:147-52. [Crossref] [PubMed]
- Elledge R, Mercuri LG, Speculand B. Extended total temporomandibular joint replacements: a classification system. Br J Oral Maxillofac Surg 2018;56:578-81. [Crossref] [PubMed]
- Elledge ROC, Higginson J, Mercuri LG, et al. Validation of an extended total joint replacement (eTJR) classification system for the temporomandibular joint (TMJ). Br J Oral Maxillofac Surg 2021;59:788-91. [Crossref] [PubMed]
- Saeed NR, Kent JN. A retrospective study of the costochondral graft in TMJ reconstruction. Int J Oral Maxillofac Surg 2003;32:606-9. [Crossref] [PubMed]
Cite this article as: Teschke M, Naujokat H. Indications for alloplastic temporomandibular joint replacement in maxillofacial surgery for benign lesions: a review of the literature and clinical cases. Front Oral Maxillofac Med 2023;5:39.

