
The efficacy of patient-fitted total joint prostheses and orthognathic surgery to reconstruct patients with congenital craniofacial deformities and temporomandibular joint malformation: a systematic review
Highlight box
Key findings
• CCD patients with TMJ malformation can be predictably treated with patient-fitted TJP and concurrent orthognathic surgery to provide stable skeletal and occlusal outcomes, improved jaw function, esthetics, and decreased pain.
• Comparative studies show patient-fitted TJP are superior to autogenous grafts (i.e., CCG and SCG) for TMJ reconstruction in CCD patients.
What is known and what is new?
• CCD patients with TMJ malformation may benefit from TMJ reconstruction and concurrent orthognathic surgery.
• Patient-fitted TJP are superior to autogenous grafts for stability and predictability of improved function, esthetics, and pain reduction.
What is the implication, and what should change now?
• TMJ patient-fitted TJP in conjunction with orthognathic surgery provides highly predictable outcomes for CCD patients with TMJ malformation. However, with the small sample size, surgeons should use caution when applying this protocol, as studies with larger subject numbers are necessary to verify this study’s outcomes.
Introduction
Background
Surgical correction of congenital craniofacial deformities (CCD) with temporomandibular joint (TMJ) malformations can be difficult to achieve acceptable functional and esthetic treatment outcomes. CCDs particularly challenging include: hemifacial microsomia (HFM), Goldenhar’s syndrome (GHS), Treacher-Collins syndrome (TCS), Nager’s syndrome (NAS), etc. Because these deformities usually have malformed or absent TMJ structures, TMJ reconstruction in conjunction with orthognathic surgery may be required to provide predictable and stable outcomes relative to function and esthetics. Autogenous bone grafts such as costochondral and sternoclavicular grafts or TMJ total joint prosthetic devices have been the primary methods for TMJ reconstruction (1-9). Realizing the anatomical, functional, and esthetic impact of the deformities, options for surgical management including TMJ reconstruction and orthognathic surgery, as well as predictability and stability of these options, will allow the surgeon to make appropriate decisions for treatment. HFM and GHS patients may benefit from unilateral TMJ reconstruction, while TCS and NAS patients may benefit from bilateral TMJ reconstruction in conjunction with orthognathic surgery (1,8,9).
Rationale and knowledge gap
Prior to the development of high-quality TMJ alloplastic patient-fitted total joint prostheses (TJP) in the early 1990’s, the standard techniques to reconstruct the TMJs in CCD patients were autogenous bone grafts including: (I) costochondral graft (CCG); (II) sternoclavicular grafts (SCG); (III) fibula grafts (vascularized); (IV) metatarsal grafts (vascularized), etc. (1). For growth center transplants, CCG or SCG have been traditionally used, but with unpredictable growth outcomes (2-7). Patient-fitted alloplastic TMJ TJP in conjunction with orthognathic surgery has provided a predictable method to reconstruct patients with end-stage TMJ pathology and CCD (8,9).
Study objective
There is controversy whether CCD patients are best treated with autogenous tissue grafts or alloplastic TMJ TJP. The purpose of this study was to perform a systematic literature review to determine the effectiveness of using TMJ patient-fitted TJP with orthognathic surgery for correcting patients with CCD and TMJ malformation. The specific aims of this study were to determine the outcomes of CCD patients surgically managed with TMJ TJP with orthognathic surgery. We present this article in accordance with the PRISMA reporting checklist (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-19/rc).
Methods
A systematic review of the literature performed identified studies related to the surgical correction of CCD patients and TMJ malformation using TMJ TJP with orthognathic surgery.
Focused question
Do TMJ TJP in conjunction with orthognathic surgery provide skeletal and occlusal stability, improve jaw function and esthetics, as well as decrease pain for CCD patients with TMJ malformation?
Search strategy
PubMed, Cochrane, Scopus, Web of Science, Ovid, and manual searches were the vehicles used to identify studies pertaining to the following MeSH filters: TMJ prosthesis AND craniofacial deformities OR hemifacial microsomia OR Goldenhar’s syndrome OR Treacher-Collins syndrome OR Nager syndrome OR congenital ankylosis OR congenital deformity OR congenital anomaly. Articles were limited to the English language. Articles were reviewed independently for inclusion by the 3 authors (LW, MK, and CH). Any conflicts for inclusion were resolved with discussion and full agreement. Dates of inclusion were from inception to December 2022.
Selection criteria
Inclusion criteria
The inclusion criteria were: (I) patients with CCD and TMJ malformation; (2) TMJ reconstruction with TJP; and (III) orthognathic surgery performed at the same or as a separate surgery.
Exclusion criteria
The exclusion criteria were: (I) CCD and TMJ malformation not present; (II) case reports; (III) technical reports; (IV) TMJ TJP were not used; and (V) orthognathic surgery was not performed concomitantly or separately.
Data extraction
Data were extracted independently by the 3 authors (LW, MK, and CH) using a previously prepared data extraction form. The following information was extracted from each study: First author; year of publication; study design; patients’ age (years); gender; sample size; populations from which patients selected; dentofacial deformities; TMJ status; surgical procedures performed; number of previous surgeries; follow-up (months); methods for outcomes measures; complications, and authors’ conclusions.
Quality assessment of studies included
A methodologic quality rating was performed by combining the proposed criteria of the Meta-Analysis of Observational Studies in Epidemiology Statement (MOSES) (10), the Strengthening the Reporting of Observational Studies in Epidemiology Statement (SROSES) (11), and the PRISMA statement (12) to verify the strength of scientific evidence in clinical decision making. A study that had all domains was classified as low risk of bias; 1 absent domain, moderate risk; and 2 or more domains absent, high risk.
Results
There is a sparsity of literature related to treatment of CCD patients with TJP and orthognathic surgery. This systematic literature review identified only 13 papers meeting the filtered requirements of TMJ TJP and CCD. Two case reports were eliminated as the 3 included patients received only mandibular TMJ components without a fossa component and without orthognathic surgery; the procedures failed in all 3 patients (13,14). Five other single case papers were excluded (15-19). One paper was excluded that included 2 cases of Treacher-Collins syndrome in a study of 14 patients receiving TJP, but the outcome data for those 2 patients were not separated from the whole group and only 4 patients from the whole group had orthognathic surgery (20). One paper was excluded where 2 of 5 patients had CCD with TMJ ankylosis treated by TJP reconstruction but no orthognathic surgery (21). Four papers met the inclusion criteria (Figure 1) (22-25). These four studies included a total of 28 patients, but one patient was removed diagnosed with idiopathic condylar resorption, and did not meet the criteria of CCD. Thus, this review includes 27 patients (Table 1) with various CCDs including: (I) HFM (n=18); (II) GHS (n=6); (III) TCS (n=1); (IV) Nager syndrome (NAS) (n=1); and (V) congenital ankylosis (CGA) (n=1).
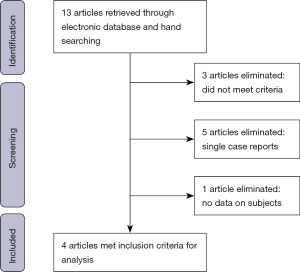
Table 1
| Study, year | No. of patients, gender | Patient type | Side operated | Age (range), years | No. previous surgeries | Surgery | Pre MIO (mm) | Post MIO (mm) | Follow-up (Months) | Complications | Post-surgery stability |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Wolford et al., 2012 (22) | 6: 2M, 4F | HFM | 6 unilat | Median 23.5 (14 to 39) | 4.3 (range, 0–12) | TMJ Con, C-SSO, MMO, Genio, TMJ FG | 36.3 (range, 2–50) | 39.2 (range, 20–45) | 75 (range, 12–132) | No comps | Very stable. No post-surg relapse |
| Polley et al., 2019 (23) | 10: 6M, 4F | HFM | 9 unilat, 1 bilat |
8–22 | NA | TMJ Con, C-SSO, MMO, FG-NA | NA | Improved | 6 to 50 | No comps for CN VII or infection | NA |
| Humphries et al., 2020 (24) | 4: 1M, 3F | 2 GH, 1 HFM, 1 CGA | 3 unilat, 1 bilat |
16 to 30 | 3 | TMJ Con, C-SSO, MMO, TMJ FG | NA; 1 Pt. 1 | 1 pt. 18 (range, 30 to 40+) | 24 | Ear canal perforation CN VII inj.-2 | NA |
| Hodzic et al., 2021 (25) | 7 | 4 GH, 1 TCS, 1 HFM, 1 NAS | NA | 20 (16 to 24) | 6 | Patient-fitted TJP-Biomet? Staged surg; TMJ and ortho surg separate; FG-NA | NA | 34 (range, 24–42) | NA | 1: infection removed-replaced; CN VII inj.-4, 2 permanent | NA |
Pre, presurgery; MIO, maximal incisal opening; M, male; F, female; HFM, hemifacial microsomia; GH, Goldenhar syndrome; CGA, congenital ankylosis; TCS, Treacher-Collins syndrome; NAS, Nager’s syndrome; unilat, unilateral; bilat, bilateral; NA, data not available; TMJ, temporomandibular joint; TMJ Con, TMJ concepts; C-SSO, contralateral sagittal split osteotomy; MMO, maxillary osteotomies; Genio, genioplasty; FG, fat graft; TJP, total joint prostheses; surg, surgery; ortho, orthognathic; Pt., patient; Comps, complications; CN, cranial nerve; inj., injury.
In three studies (22-24), TMJ Concepts TJP (TMJ Concepts Inc. Ventura, CA, USA) were used in the TMJ reconstruction. One study (25) did not identify the prostheses, but it appears that at least one patient received a Biomet Microfixation (Biomet, Inc., Jacksonville, FL, USA) TJP based on an included figure, but all prostheses used were patient-fitted (Table 1).
Three studies (22-24) identified gender with 9 males and 11 females, whereas one study (25) with 7 patients did not identify gender. Three studies (22-24) indicated the surgical side for the TJP with 18 unilateral and 2 bilateral. One study (25) with 7 patients did not indicate unilateral or bilateral TJP. However, in this study, one patient had TCS and one had NAS, which usually requires bilateral TJP. Wolford et al. (22) recorded the average surgery age of 23.5 years (range, 14 to 39 years); Polley et al. (23) range of 8 to 22 years; Humphries et al. (24) range of 16 to 30 years; and Hodzic et al. (25) average 20 years (range, 16 to 24 years) (Table 1).
Wolford et al. (22) provided the only study reporting the mean presurgery maximum incisal opening (MIO) 36.3 mm and post-surgery MIO 39.2 mm. Polley et al. (23) only reported post-surgery MIO was improved. Humphries et al. (24) stated the post-surgery MIO was 30 to 40+ mm. Hodzic et al. (25) reported average post-surgery MIO of 34 mm (range, 24–42 mm). Wolford et al. (22) reported follow-up mean of 75 months (range, 12 to 132 months), Polley et al. (23) 6 to 50 months, Humphries et al. (24) 24 months, and Hodzic et al. (25) did not record follow-up time. Wolford et al. (22) Humphries et al. (24), and Hodzic et al. (25) recorded the number of previous surgeries at 4.3, 3, and 6 respectively. Wolford et al. (22), Polley et al. (23), and Humphries et al. (24) reported surgery to include unilateral TMJ TJP, contralateral mandibular ramus osteotomy, and maxillary osteotomies. Two studies Wolford et al. (22) and Humphries et al. (24) reported placing fat grafts around the prostheses at surgery, while Polley et al. (23) and Hodzic et al. (25) did not provide evidence of using fat grafts (Table 1).
Only Wolford et al. (22) documented long-term stability showing no relapse by cephalometric analysis. Three studies Wolford et al. (22), Humphries et al. (24), and Hodzic et al. (25) reported complications. Wolford et al. (22) reported no significant post-surgery complications. Humphries et al. (24) reported one patient had an ear canal perforation and 2 patients had cranial nerve (CN) VII injury. Hodzic et al. (25) reported one patient had an infection of the prosthesis requiring removal and later replacement. Four of 7 patients had CN VII injury with 2 having permanent damage. Polley et al. (23) did not include complications (Table 1). Only Wolford et al. (22) presented subjective outcome data on TMJ pain, headaches, diet, jaw function, and disability, where all patients improved or remained the same.
Quality assessment of included studies
Wolford et al. (22) had low risk of bias as all domains were included. Polley et al. (23), Humphries et al. (24), and Hodzic et al. (25) were at high risk of bias, with 2 or more domains missing. The details of critical appraisal are presented in Table 2.
Table 2
| Author | Year | Study population clearly described | Defined inclusion and exclusion criteria | Interventions clearly described | Loss of follow up | Clearly defined and valid outcome measures | Statistical analysis | Estimated risk of bias |
|---|---|---|---|---|---|---|---|---|
| Wolford et al., (22) | 2012 | Yes | Yes | Yes | Yes | Yes | Yes | Low |
| Polley et al., (23) | 2019 | Yes | No | Yes | Yes | No | No | High |
| Humphries et al., (24) | 2020 | Yes | Yes | Yes | Yes | No | No | High |
| Hodzic et al., (25) | 2021 | Yes | No | No | Yes | No | No | High |
Study reviews
Wolford et al. (22) in 2012 introduced the protocol for treating non-growing HFM patients with unilateral TMJ TJP and orthognathic surgery in a single surgical stage (Table 3). This is the only study that looked at subjective and objective outcomes. Six patients (4 females, 2 males) were treated using the surgical protocol, average age was 23.5 years (range, 14 to 39 years), with a follow-up average of 75 months (range, 12 to 132 months). All patients received unilateral TMJ Concepts TJP and fat grafts packed around the articulating area of the TJP. Presurgery, two patients (33%) had contralateral disc displacement repaired at the same surgery with the Mitek anchor technique. Patients were evaluated subjectively for pain, diet, jaw function, and disability using the Likert numerical analog scale (0 to 10), before surgery and at longest post-surgery follow-up. Lateral cephalometric radiographs from presurgery, immediately post-surgery, and at longest follow-up were used to determine surgical changes and post-surgical stability. All patients improved or remained unchanged relative to the subjective parameters. Incisal opening increased 2.9 mm from 36.3 to 39.2 mm. Predictably, the excursion movements for the TJP side decreased. Counterclockwise rotation, advancement, and transverse leveling was surgically performed on the maxillo-mandibular complex. The mean anterior horizontal surgical movement of the anterior nasal spine (ANS) was 1.3 mm, upper incisor tip (U1T) 7.4 mm, lower incisor tip (L1T) 8.9 mm, point B 14.8 mm, pogonion (Pog) 18.6 mm, and menton (Me) 17.5 mm. The mean decrease of the occlusal plane angle (OPA) was −12.3°. Long-term analysis of post-surgical stability showed posterior movement of Point A and U1T of 1 mm. The mandibular anatomical points and OPA remained very stable with no significant change. No significant complications were identified.
Table 3
| 1. Disc reposition on contralateral side if displaced (Mitek anchor technique). |
| 2. Ipsilateral condylectomy and coronoidectomy via endaural or preauricular incision. |
| 3. Ipsilateral submandibular incision with release of masseter and medial pterygoid muscle. |
| 4. Ipsilateral mandible mobilization via submandibular incision. |
| 5. Contralateral mandibular ramus sagittal split osteotomy. |
| 6. Counterclockwise rotation of the mandible, intermediate splint, MMF. |
| 7. Contralateral mandibular ramus rigid fixation, close incision. |
| 8. TMJ Concepts total joint prosthesis placement in ipsilateral side. |
| 9. Reattach masseter muscle on ipsilateral side, close submandibular incision. |
| 10. Harvest fat graft from abdomen and pack around articulation area of prosthesis. |
| 11. Endaural or preauricular incision closure. |
| 12. Maxillary osteotomies, mobilization, segmentation, palatal splint if indicated. |
| 13. Partial turbinectomies, nasoseptoplasty, etc. if indicated. |
| 14. MMF, maxillary stabilization with bone plates, bone or synthetic bone grafting. Close incision. |
| 15. MMF removed, apply light elastics. |
| 16. Other indicated procedures (genioplasty, rhinoplasty, facial augmentation, etc.). |
CCD, congenital craniofacial deformity; MMF, maxillo-mandibular fixation; TMJ, temporomandibular joint.
Polley et al. (23) in 2019 reported a multi-institutional study including ten HFM patients, six males and four females, age range 8 to 22 years. Nine patients had unilateral, and one patient had bilateral TJPs. Follow-up ranged from 6 to 50 months. No data were provided relative to number of previous surgeries nor presurgical and postsurgical incisal opening. The authors state MIO was maintained or improved. No cephalometric analysis data was provided for surgical change and stability, nor subjective evaluation of pain, diet, jaw function, or disability. The authors stated results were stable. TMJ Concepts TJP were used in all cases but no report of fat grafts around the TMJ TJP. The TMJ and orthognathic surgery were performed in a single stage. Post-surgery complications were not reported.
Humphries et al. (24) in 2020, reported on five patients, age range 16 to 30 years, with average follow-up of 24 months. There were two GHS, one HFM, and one CGA. One patient diagnosed with TMJ idiopathic condylar resorption was removed from the study as that patient did not meet the inclusion criteria for CCD, so only 4 patients, 3 females and 1 male, were included. The patients averaged three prior surgeries. Although orthognathic surgery was performed concomitantly with the TMJ reconstruction, the surgical changes were relatively small with advancement at Point A 1.18 mm, Point B 4.66 mm, genial tubercle 4.96 mm, and menton 5.87 mm. No cephalometric analysis of long-term post-surgical stability was performed. TMJ Concepts TJP were used in all patients with fat grafts around the TJP. Patients were reported to have improved occlusions. Although presurgery MIO was not reported for 3 patients, post-surgery MIO was greater than 30 mm. The patient with CGA had presurgical MIO of 1 mm and post-surgery improved to 18 mm. Complications included an ear canal perforation and two of the patients had CN VII injuries; one with improvement and one permanent.
Hodzic et al. (25) in 2021, presented 7 patients average age 20 years (range, 16 to 24 years), but no length of follow-up recorded. The study included four GHS, one TCS, one NAS and one HFM. It was not recorded if TMJ TJP were done unilateral or bilateral, but it would be assumed that the TCS and NAS were likely performed bilaterally and the other 5 patients unilaterally. The patients had an average of six previous surgeries. Four of the seven patients had bimaxillary orthognathic surgery performed a few months to years prior to the TMJ TJP procedure. The prostheses used were not identified, and there was no documentation of fat grafts used. There were no presurgery MIOs recorded but post-surgery the average MIO was 34 mm. Complications included one infection case that required removal and then replacement of the TMJ prosthesis. Four of the seven patients had CN VII damage with two permanent.
Discussion
The key findings of this study and the included comparative studies of TMJ TJP versus autogenous grafts for TMJ reconstruction in the CCD patient are included in Highlight box. This systematic literature review identified studies that evaluated the outcomes of CCD patients with TMJ malformation treated with TMJ TJP and orthognathic surgery. The literature is sparse and only 4 studies met the inclusion criteria. The studies have small numbers of subjects ranging from 4 to 10, for a total of 27 CCD patients available for outcome analysis. The 4 studies included 5 different CCD anomalies: HFM (n=18), GHS (n=6), TCS (n=1), NAS (n=1), and CGA (n=1). Three of the studies (23-25) are descriptive of outcomes and do not provide data relative to stability or subjective outcomes. These studies report post-surgery MIO outcomes that are acceptable, but do not provide the presurgical MIOs for comparison. All four studies reported stable outcomes, but only Wolford et al. (22) provided cephalometric data on surgical change, long term surgical stability, as well as subjective and objective outcomes. Stability outcomes showed no statistically significant relapse of mandibular anatomical landmarks (Point B, Pogonion, Menton, lower incisor tips, occlusal plane). There were significant improvements in TMJ pain, headaches, jaw function (except excursion movements), diet and disability. The results of these 4 studies document the predictable outcomes for the CCD patients treated with TMJ TJP and orthognathic surgery. There are 5 different CCD anomalies included. These CCDs have been described in the literature along with the genetic factors, occurrence, clinical and imaging features, etc. (6,8,9,22,25,26), so that information will not be re-iterated.
Strengths and limitations
Strengths of this study indicate the use of TMJ TJP and orthognathic surgery can provide predictable outcomes for CCD patients relative to stability, improved jaw function, and decrease in pain. Limitations of this study include: (I) small sample of papers (n=4) meeting the inclusion criteria; (II) small number of patients in each study (n=27 patients from all 4 studies); and (III) three of the 4 studies did not include stability nor subjective outcome data. There is a significant need for additional studies with larger populations to further verify the outcomes documented in these included studies.
Patient-fitted TMJ TJP
TMJ Concepts patient-fitted TJP and Biomet Microfixation stock TJP are the only Federal Drug Administration (FDA) approved systems in the USA for TMJ reconstruction. Considering application to CCD patients, patient-fitted TJP is superior to a stock TJP for TMJ reconstruction and concomitant orthognathic surgery (8,9,22).
Biomet Microfixation system
The Biomet Microfixation stock TMJ TJP system has several sizes of fossa and mandibular components to choose from. Biomet patient-fitted devices are available in other countries, but are not FDA approved for use in the USA. There are 3 lengths available for the stock ramus component including: 45, 50, and 55 mm which limits CCD patient application. There are three fossa component sizes (small, medium, and large), composed of dense ultra-high molecular weight polyethylene (UHMWPE). Concerns with the fossa design is there is no osseo-integration of the fossa component and no posterior stop in the fossa to provide a predictable centric relation position of the condyle, rendering the standard stock prosthesis unsuitable for reconstruction of the CCD patients that also require orthognathic surgery. Good outcomes have been reported in the literature using the stock device for indicate TMJ pathology (27-32), but not for the surgical requirements of the CCD patients. The fossa component of the patient-fitted prosthesis does have a posterior stop, but no osseo-integration. Absence of the zygomatic arch and glenoid fossa in some CCD patients may require the fossa component to be attached to the temporal bone. The stock fossa component is not applicable, and the patient-fitted fossa device may not be suitable because of potential screw loosening related to the thin temporal bone, lateral slope of the temporal bone, and lack of osseointegration of the fossa component.
TMJ concepts system
The TMJ Concepts patient-fitted TMJ TJP devices are designed on a 3-D stereolithic model where the mandible and maxilla have been placed into their final surgical position by virtual surgical planning (VSP), and TMJ components manufactured to meet the patient’s specific anatomical requirements. A commercially pure titanium (CPT) shell with 4 layers of CPT mesh bonded to the shell is fitted to the fossa contour. The functional articulating surface of UHMWPE is bonded to the titanium mesh to complete the fossa component. Screw fixation of the fossa component to the lateral rim of the fossa or to the temporal bone (HFM patients) provides osseointegration of the CPT mesh framework maximizing the long-term stability of the fossa component. The posterior stop of the fossa component is necessary as the stop provides a centric relation position for the condylar head of the mandibular component. Titanium alloy is used for the mandibular ramus component and cobalt-chromium-molybdenum (Co-Cr-Mo) alloy is used for the condylar head. The titanium alloy provides osseo-integration of the mandibular component to the ramus. The gold standard in orthopedics is a Co-Cr-Mo condylar head functioning against a polyethylene fossa. The ability to reconstruct the TMJ and advance the mandible, as well as perform concomitant orthognathic surgery at the same operation, is provided with the TMJ Concepts TJP system. The outcome stability has been well documented in the literature (33-42).
Age of surgical intervention
When considering alloplastic TJP for CCD patients, waiting until jaw growth is relatively complete, will improve outcome predictability and limit surgical correction to one major operation particularly for patients requiring unilateral TJP. By the age of 15 years, females commonly have most of their facial growth complete (98%), and by the age of 17 to 18 years for males (43). A common component of CCD patients (i.e., HFM, GHS) is asymmetric growth that may require orthognathic surgical procedures that may have additional unfavorable effects on subsequent facial growth (44-47). The contralateral side of the mandible of the HFM patients will usually have a normal growing condyle and mandible that rarely requires TMJ reconstruction. Waiting until growth of the contralateral condyle is complete will provide predictable long-term treatment outcomes in a single operation. Unilateral TJP, with or without orthognathic surgery performed during growth may result in redevelopment of asymmetry, antero-posterior discrepancy and malocclusion that may develop during the completion of growth, as the ipsilateral mandible will not grow, but the contralateral side will grow normally, possibly requiring additional surgery at a later time for correction. Surgery before growth is complete may be required for masticatory dysfunction, airway obstruction, sleep apnea, psychological factors, etc., but a TJP may be the preferred option with follow-up orthognathic surgery. Wolford et al. (44-47) have previously published age consideration guidelines for orthognathic and TMJ surgical procedures since there are adverse effects of performing these surgeries during growth.
Surgical intervention can be done earlier for CCD patients requiring bilateral TJP for TMJ reconstruction using patient-fitted TJP and orthognathic surgery; 13–14 years in females and 15–16 years of age in males. Post-surgical growth will be predominately in a vertical vector with maxillo-mandibular complex rotating downward and backward as the residual alveolar bone growth of the maxilla and mandible is completed. The occlusion should remain stable (8,9,44-47).
Autogenous tissue grafts
Until the development of a predictable and safe patient-fitted TMJ TJP in the early 1990’s, TMJ reconstruction used autogenous bone grafts, specifically CCG and SCG. Autogenous bone grafts have advantages including: (I) use of native bone; (II) CCG and SCG can provide growth potential; (III) fibula and metatarsal vascularized grafts are available; and (IV) SCG can provide an attached articular disc (1). Autogenous bone grafts have disadvantages including: (I) operating time significantly increased with requirement for graft harvest; (II) donor site morbidity; (III) physiological loading of grafts can cause bone remodeling/resorption, bending, warping, and fracture; (IV) correction of significant CCD deformities unpredictable; (V) CCG and SCG growth unpredictable; (VI) occlusion control difficulty; and (VII) TMJ ankylosis risk (1).
Therefore, indications for condylar replacement using bone grafts include the following: (I) free grafts applicable with 0 to 1 previous TMJ surgeries; (II) free grafts with good vascular bed; (III) vascularized fibula grafts when hard and soft tissue grafting required; (IV) CCG and SCG for growth center transplant if indicated; (V) patient-fitted TJP unavailable; (VI) patient prefers autogenous tissues over alloplastic TJP; (VII) metal hypersensitivity to TJP metals; and (VIII) minimal repositioning of the dento-skeletal structures required (1).
Free bone graft contraindications include: (I) two or more previous TMJ surgeries; (II) TMJs involved in inflammatory or connective tissue autoimmune disease; (III) presence of TMJ autogenous graft or alloplastic implant failure; (IV) decreased vascularization, or prolonged healing conditions, etc.; (V) polyarthropathies; and (VI) requirement for significant movement of the dento-skeletal structures with TMJ reconstruction and orthognathic surgery. Autogenous tissue grafts provide unpredictable outcomes when applied to TMJ reconstruction alone or in conjunction with orthognathic surgery (1).
Patient-fitted TMJ TJP
Advantages of patient-fitted TJP include: (I) prosthesis is designed to fit the anatomical requirements with the mandible and maxilla in the final position; (II) mandible can be advanced, and ramus vertically lengthened with the prosthesis; (III) major dento/craniofacial deformities can be predictably corrected; (IV) fossa component has a defined posterior stop, which is a key component for stability when combining TMJ and orthognathic surgery; (V) fossa and ramus components osseo-integrate; (VI) at the same operation, the TMJ and orthognathic surgery can be performed; (VII) prosthesis works in a poorly vascularized recipient bed; (VIII) VSP surgical planning and manufacturing of the patient-fitted prostheses aided with construction of 3-D stereolithic model; and (IX) long-term function and stability. Disadvantages include: (I) presurgical preparation time required for stereolithic model construction; (II) patient -fitted devices take time to manufacture; (III) alloplastic materials; (IV) highly sensitized patients may express metal hypersensitivity reaction to the TJP metals; (V) surgical risks associated with TMJ reconstruction; and (VI) TMJ TJP functional service life is unknown (1).
Periarticular fat grafts
TMJ reconstruction with autogenous bone grafts or alloplastic TJP is subject to the development of fibrosis and heterotopic/reactive bone around the articulating areas resulting in functional impairment and pain. Fat grafts packed around the articulating areas of the TMJ TJP significantly improves the treatment outcomes for the following reasons: (I) dead space around the articulating areas is eliminated; (II) blood clot forming around the grafts or TJP is eliminated; (III) bone growth and fibrosis is inhibited; (IV) pain is decreased; and (V) TMJ function improved (48-50).
Wolford et al. (48-50) and Mercuri et al. (51) have previously reported on the use of fat grafts packed around the articulating area of the TJP, harvested from the abdomen or buttock. The post-surgical incidence of peri-implant fibrosis and heterotopic/reactive bone formation is significantly reduced. Patients receiving fat grafts compared to those without fat grafts, had significantly better outcomes for pain and increased jaw function compared to those without fat grafts. Approximately 35% of patients without fat grafts developed dense fibrosis and/or heterotopic/reactive bone around the TJP, requiring additional surgery for removal and placement of fat grafts. Reoperation has been decreased to less than 2% for heterotrophic bone and fibrosis with the use of fat grafts (52,53). Wolford also described the use of fat grafts on the ipsilateral side of the face to augment the deficient soft tissues in HFM patients (54).
Autogenous bone grafts versus alloplastic TMJ TJP: comparative studies
Studies comparing autogenous tissues versus TJP for TMJ reconstruction are scarce. The Henry and Wolford study in 1994 (55), evaluated 107 patients exposed to Proplast Teflon implants (Vitek, Inc., Houston, TX, USA) with TMJ reconstruction. The study compared TMJ reconstruction outcomes of using TJP or various autogenous tissue grafts (CCG, SCG, ear cartilage, dermal, temporal muscle/fascia grafts, etc.). The autogenous tissue grafts had high failure rates with only 8% to 31% successful outcomes. The Techmedica TJP had an 86% success rate.
Freitas, Mehra, Wolford (56) in 2002, compared CCG, SCG, and TJP for TMJ reconstruction in rheumatoid arthritis. Better objective and subjective outcomes were achieved with the TJP compared to the autogenous tissues. There was significantly reduced operating time with the TJP, and significantly better skeletal and occlusal stability with maxillo-mandibular advancements.
Wolford, McPhillips, Rodrigues (57) in 2009, evaluated outcomes of patient with TMJ ankylosis using CCG, SCG, and TJP. No fat grafts were placed around the CCG and these cases re-ankylosed. A third of the SCG did not have fat grafts and re-ankylosed. Two-thirds of the patients with SCG had fat grafts placed around the articulating area of the grafts with no recurrence of ankylosis. All patients that received the TJP had fat placed around the articulating area with no re-ankylosis nor mandibular relapse, and substantial improvement of jaw function.
Saeed et al. (58) in 2002, performed an outcome study of CCG compared to TJP for TMJ reconstruction. There was a significantly greater rate of reoperation following CCG (55% of the patients) versus 12% who received TJP. The TJP patients had better objective and subjective outcomes.
Mehra et al. (59) in 2018 evaluated outcomes for patients with autoimmune or connective tissue diseases (rheumatoid, lupus or psoriatic arthritis) treated with autogenous bone grafts (CCG or SCG) Group 1 (n=9) compared to TJP (TMJ Concepts) Group 2 (n=20). Maxillary osteotomies were performed on two-thirds of the subjects. Group 1 had an average mandibular advancement relapse of 32% at Point B, whereas Group 2 average relapse was 5%. These studies (55-59) demonstrated that TJP provide significantly better stability compared to autogenous grafts for TMJ reconstruction.
Surgical management of CCD patients with TMJ malformation
Reconstructing the TMJs and advancing the maxillo-mandibular complex in a counter-clockwise direction with the affected side(s) treated with a patient-fitted TJP with orthognathic surgery provides predictable treatment outcomes functionally and esthetically for CCD patients with TMJ malformation (1,8,9,22). Other adjunctive procedures (turbinectomies, nasoseptoplasty, genioplasty, rhinoplasty, etc.) may be indicated. Depending on the surgeon’s skills and preference, the procedures can be done at one operation, or divided into 2 or more operations. Secondary bony and soft tissue procedures may be indicated to eliminate residual deficiencies such as bone grafts, synthetic bone, alloplastic implants, etc. to build up the remaining deficient skeletal structures and soft tissue augmentation to correct soft tissue defects using fat grafts, soft tissue procedures, tissue flaps, free vascularized grafts, and so on (1,22,54).
Virtual surgical planning (VSP)
VSP is a computer generated 3-D model of the patient’s anatomy with the ability to reposition the jaws and occlusion into a predetermined final position. The repositioned mandible and maxilla on the computer model, is transferred into the 3-D stereolithic model (60,61). The TMJ Concepts TJP are designed and manufactured from the stereolithic model. Approximately two weeks prior to surgery, final dental models are acquired, prepared and forwarded to the VSP company, where the dental models are incorporated into the computer model. Segmentalization of the maxilla can be completed virtually on the computer model as well as construction of the intermediate and the final palatal splints.
Surgical protocol
The surgical protocol and sequencing used by the authors for treating CCD patients requiring unilateral TMJ TJP and orthognathic surgery is outlined in Table 3. The best functional and esthetic outcomes for these cases include counter-clockwise rotation of the maxillo-mandibular complex (1,22,37,42,60,61). The ipsilateral TMJ TJP reconstruction and contralateral sagittal split osteotomy are performed first to reposition the mandible. This simplifies model surgery and splint construction and improves the accuracy of the patient’s surgery and outcome (60,61). Counter-clockwise rotation of the mandible creates posterior open bites being greater on the ipsilateral side as the transverse cant of the mandibular occlusal plane is corrected. Maxillary segmentation requires a palatal splint to stabilize the upper arch, while allowing maximum interdigitation of the occlusion, as the maxilla is repositioned and stabilized (1,22,37,42,60,61).
The surgical sequencing for the CCD patients requiring bilateral TMJ TJP is outlined in Table 4. Counterclockwise rotation of the maxillo-mandibular complex can maximize the functional and esthetic outcomes, create a normal oropharyngeal airway dimension, correcting sleep apnea issues that are common with these patients. Repositioning the mandible first with the TMJ TJP in the surgical sequencing, followed by the maxillary osteotomies, provides a more predictable outcome. The specifics of the surgical protocols for unilateral and bilateral TJP for CCD patients has been previously published in detail and will only be briefly re-iterated here (1,22,37,60,61).
Table 4
| 1. Bilateral mandibular condylectomy and coronoidectomy (Endaural or preauricular incision). |
| 2. Submandibular incision, detach masseter and medial pterygoid muscles. |
| 3. Mobilize mandible with counter-clockwise rotation. |
| 4. Placement of intermediate splint, MMF. |
| 5. Bilateral TMJ Concepts total joint prosthesis placement. |
| 6. Reattach masseter muscles, close submandibular incisions. |
| 7. Harvest fat graft from abdomen and pack around articulation area of prostheses. |
| 8. Endaural or preauricular incision closure. |
| 9. Maxillary osteotomies, mobilization, segmentation, palatal splint if indicated. |
| 10. Partial turbinectomies, nasoseptoplasty, etc., if indicated. |
| 11. MMF, maxillary stabilization with bone plates, bone or synthetic bone grafting. Close incision. |
| 12. MMF removed, place light elastics. |
| 13. Other indicated procedures (genioplasty, rhinoplasty, facial augmentation, etc.). |
CCD, congenital craniofacial deformity; MMF, maxillo-mandibular fixation; TMJ, temporomandibular joint.
Sleep apnea is common in CCD patients resulting from retruded mandible, decreased oropharyngeal airway and/or nasal airway obstruction. Advancement of the maxillo-mandibular complex with counter-clockwise rotation is highly effective for increasing the oropharyngeal airway dimensions. Partial nasal turbinectomies and nasoseptoplasty may be required to eliminate nasal airway obstruction. Post-surgery these patients should have considerable improvement in the airway and eliminate sleep apnea (1,22,42,62-65).
The longevity of the TMJ Concepts TJP is not yet known. Mercuri et al. (34,35) in 1995 and 2002 reported multicenter studies with multiply operated TMJ patients reconstructed with the TMJ Concepts TJP. There were statistically significant positive changes in many subjective and objective evaluations post-surgery. Wolford et al. (36) in 2003 published a study on 36 patients with 65 TMJs reconstructed with the Techmedica/TMJ Concepts TJP with a 5- to 8-year follow-up. The long-term post-surgical occlusal and skeletal stability success rate was 90%, and pain reduction in 89% of patients.
In 2009, a series of paper were published (37,62,66) using TMJ Concepts TJP and concomitant orthognathic surgery with counter-clockwise rotation of the maxillo-mandibular complex. The same population of 47 females with an average follow-up of 40.6 months were included in all 3 studies. Part I of the series (37) evaluated skeletal and occlusal surgical changes and long-term post-surgical skeletal stability. The surgical change of the mandible at pogonion was an average advancement of 18 mm and the occlusal plane was decreased an average of 15°. The skeletal and occlusal structures remained stable at longest follow-up, with no statistically significant changes. Part II of the series documented a significant increase in the dimensions of the oropharyngeal airway (62).
In Part III of the series (66), long-term outcomes were evaluated for pain and jaw function for the same patient group. Twenty-two of the 47 patients had multiple previous failed TMJ surgeries. The results showed statistically significant improvement for facial pain/headache, TMJ pain, jaw function, diet, and disability. Significantly better outcomes were experienced by patients that had 0 to 1 previous TMJ surgeries compared to patients with 2 or more previous TMJ surgeries. These results are consistent with Wolford et al. (22) HFM study with statistically significant improvement in all subjective parameters.
Wolford et al. (41) published a 20-year follow-up study documenting the long-term stability and function of the Techmedica/TMJ Concepts TJP. There were 56 patients available for long-term follow-up evaluation, with all patients functioning on their original prostheses. Incisal opening improved by 7 mm, pain decreased 4 points (on a 0 to 10 Likert numerical scale), ability to chew improved 5 points, while 86% reported significant improvement in quality of life, 11% remained the same and 3% reported that they were worse than prior to surgery. This study demonstrates the long-term quality outcomes using this prosthesis system.
Conclusions
Through the years, various options have been proposed for surgical correction of CCD patients with TMJ malformations. CCG and SCG are the most popular autogenous bone grafts used to treat unilateral or bilateral mandibular/condylar hypoplasia or aplasia. Autogenous bone grafts are unreliable to provide predictable surgical outcomes relative to skeletal and occlusal stability, function, and pain, as excessive over-growth or relapse can be expected related to graft flexibility, extended healing time, resorption, fracture, ankylosis, and biological effects of graft loading and response.
TMJ Concepts patient-fitted TJP combined with orthognathic surgery is the preferred option for surgical treatment of CCD patients requiring unilateral or bilateral TMJ TJP in conjunction with orthognathic surgery because: (I) no bone graft donor site, decreasing morbidity and operating time; (II) highly predictable outcomes relative to stability, TMJ and occlusal function, esthetics, and decrease in pain; (III) does not require bony reconstruction of glenoid fossa; (IV) TMJ Concepts fossae and mandibular components osseo-integrate providing reliable long-term stability; and (V) TMJ Concepts, TJP is a patient-fitted device to meet the patient’s specific anatomical requirements for mandibular advancement, vertical lengthening and TMJ reconstruction. TMJ Concepts patient-fitted TJP combined with orthognathic surgery, appears to be the preferred technique for the surgical correction of CCD patients with TMJ malformation, but because of the small sample size, surgeons should use caution with this surgical approach. Additional research is necessary to further validate these treatment protocols and outcomes.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Louis Mercuri) for the series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-19/rc
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-19/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-19/coif). The series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wolford L. Part III; Chapter 8: Autogenous tissues versus alloplastic TMJ condylar replacement. In Connelly S, Tartaglia G, Silva R (eds.). Contemporary management of temporomandibular disorders. Springer, 2019:173-202.
- Kaban LB, Moses MH, Mulliken JB. Surgical correction of hemifacial microsomia in the growing child. Plast Reconstr Surg 1988;82:9-19. [Crossref] [PubMed]
- Ware WH, Brown SL. Growth centre transplantation to replace mandibular condyles. J Maxillofac Surg 1981;9:50-8. [Crossref] [PubMed]
- Peltomäki T, Quevedo LA, Jeldes G, et al. Histology of surgically removed overgrown osteochondral rib grafts. J Craniomaxillofac Surg 2002;30:355-60. [Crossref] [PubMed]
- Munro IR, Phillips JH, Griffin G. Growth after construction of the temporomandibular joint in children with hemifacial microsomia. Cleft Palate J 1989;26:303-11. [PubMed]
- Mulliken JB, Ferraro NF, Vento AR. A retrospective analysis of growth of the constructed condyle-ramus in children with hemifacial microsomia. Cleft Palate J 1989;26:312-7. [PubMed]
- Wolford LM, Cottrell DA, Henry C. Sternoclavicular grafts for temporomandibular joint reconstruction. J Oral Maxillofac Surg 1994;52:119-28; discussion 128-9. [Crossref] [PubMed]
- Wolford LM, Perez DE. Surgical management of congenital deformities with temporomandibular joint malformation. Oral Maxillofac Surg Clin North Am 2015;27:137-54. [Crossref] [PubMed]
- Wolford L. Surgical management of hemifacial microsomia with temporomandibular joint malformation. Chapter 6. In: Yates D, Markiewicz M (eds.). Craniofacial microsomia and Treacher Collins Syndrome: Comprehensive treatment of associated facial deformities. Switzerland AG: Springer Nature, 2022:93-131.
- Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008-12. [Crossref] [PubMed]
- von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol 2008;61:344-9. [Crossref] [PubMed]
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. [Crossref] [PubMed]
- Wittbjer J, Sarnäs KV, Rune B. Displacement of the mandible in a child with congenital unilateral temporomandibular joint ankylosis treated with two-stage condylar replacement: a long-term study with the aid of roentgen stereometric analysis. Cleft Palate Craniofac J 2001;38:636-44. [Crossref] [PubMed]
- Clauser LC, Consorti G, Elia G, Tieghi R, Galiè M. Management of temporomandibular joint reankylosis in syndromic patients corrected with joint prostheses: surgical and rehabilitation protocols. Craniomaxillofac Trauma Reconstr 2014;7:71-78. [Crossref] [PubMed]
- Schlieve T, Almusa M, Miloro M, et al. Temporomandibular joint replacement for ankylosis correction in Nager syndrome: case report and review of the literature. J Oral Maxillofac Surg 2012;70:616-25. [Crossref] [PubMed]
- Zanakis NS, Gavakos K, Faippea M, et al. Application of custom-made TMJ prosthesis in hemifacial microsomia. Int J Oral Maxillofac Surg 2009;38:988-92. [Crossref] [PubMed]
- Farzad P. Reconstruction of nongrowing hemifacial microsomia patient with custom-made unilateral temporomandibular joint total joint prosthesis and orthognathic surgery. J Oral Biol Craniofac Res 2017;7:62-6. [Crossref] [PubMed]
- Cascone P, Vellone V, Ramieri V, et al. Reconstruction of the Adult Hemifacial Microsomia Patient with Temporomandibular Joint Total Joint Prosthesis and Orthognathic Surgery. Case Rep Surg 2018;2018:2968983. [Crossref] [PubMed]
- Salman NJ, Pimenta E, Souza D, Kuriki E, et al. A patient with Camurati-Engelmann disease presenting bilateral TMJ ankylosis; A case report. Int J Surg Case Rep 2020;74:144-7. [Crossref] [PubMed]
- Keyser BR, Banda AK, Mercuri LG, et al. Alloplastic total temporomandibular joint replacement in skeletally immature patients: a pilot survey. Int J Oral Maxillofac Surg 2020;49:1202-9. [Crossref] [PubMed]
- Sinn DP, Tandon R, Tiwana PS. Can Alloplastic Total Temporomandibular Joint Reconstruction be Used in the Growing Patient? A Preliminary Report. J Oral Maxillofac Surg 2021;79:2267.e1-2267.e16. [Crossref] [PubMed]
- Wolford LM, Bourland TC, Rodrigues D, et al. Successful reconstruction of non-growing hemifacial microsomia patients with unilateral temporomandibular joint total joint prosthesis and orthognathic surgery. J Oral Maxillofac Surg 2012;70:2835-53. [Crossref] [PubMed]
- Polley JW, Girotto JA, Fahrenkopf MP, et al. Salvage or Solution: Alloplastic Reconstruction in Hemifacial Microsomia. Cleft Palate Craniofac J 2019;56:896-901. [Crossref] [PubMed]
- Humphries LS, Shakir A, Figueroa AA, et al. Custom Alloplastic Temporomandibular Joint Reconstruction: Expanding Reconstructive Horizons. J Craniofac Surg 2020;31:1651-8. [Crossref] [PubMed]
- Hodzic Z, Tornwall J, Leikola J, et al. Alloplastic temporomandibular reconstruction in congenital craniofacial deformities. J Craniofac Surg 2021;32:e548-e551. [Crossref] [PubMed]
- Gorlin RJ, Cohen MM Jr, Hemekam RCM. Syndromes of the head and neck (4th Edition). Oxford Universe Press, 2001:790-7.
- Giannakopoulos HE, Sinn DP, Quinn PD. Biomet Microfixation Temporomandibular Joint Replacement System: a 3-year follow-up study of patients treated during 1995 to 2005. J Oral Maxillofac Surg 2012;70:787-94; discussion 795-6. [Crossref] [PubMed]
- Machon V, Hirjak D, Beno M, et al. Total alloplastic temporomandibular joint replacement: the Czech-Slovak initial experience. Int J Oral Maxillofac Surg 2012;41:514-7. [Crossref] [PubMed]
- Aagaard E, Thygesen T. A prospective, single-centre study on patient outcomes following temporomandibular joint replacement using a custom-made Biomet TMJ prosthesis. Int J Oral Maxillofac Surg 2014;43:1229-35. [Crossref] [PubMed]
- Leandro LF, Ono HY, Loureiro CC, et al. A ten-year experience and follow-up of three hundred patients fitted with the Biomet/Lorenz Microfixation TMJ replacement system. Int J Oral Maxillofac Surg 2013;42:1007-13. [Crossref] [PubMed]
- Westermark A. Total reconstruction of the temporomandibular joint. Up to 8 years of follow-up of patients treated with Biomet((R)) total joint prostheses. Int J Oral Maxillofac Surg 2010;39:951-5. [Crossref] [PubMed]
- Sanovich R, Mehta U, Abramowicz S, et al. Total alloplastic temporomandibular joint reconstruction using Biomet stock prostheses: the University of Florida experience. Int J Oral Maxillofac Surg 2014;43:1091-5. [Crossref] [PubMed]
- Wolford LM, Cottrell DA, Henry CH. Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J Oral Maxillofac Surg 1994;52:2-10; discussion 11. [Crossref] [PubMed]
- Mercuri LG, Wolford LM, Sanders B, et al. Custom CAD/CAM total temporomandibular joint reconstruction system: preliminary multicenter report. J Oral Maxillofac Surg 1995;53:106-15; discussion 115-6. [Crossref] [PubMed]
- Mercuri LG, Wolford LM, Sanders B, et al. Long-term follow-up of the CAD/CAM patient fitted total temporomandibular joint reconstruction system. J Oral Maxillofac Surg 2002;60:1440-8. [Crossref] [PubMed]
- Wolford LM, Pitta MC. TMJ Concepts/Techmedica custom-made TMJ total joint prosthesis: 5-year follow-up. Int J Oral Maxillofac Surg 2003;32:268-274. [Crossref] [PubMed]
- Dela Coleta KE, Wolford LM, Gonçalves JR, et al. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part I--skeletal and dental stability. Int J Oral Maxillofac Surg 2009;38:126-38. [Crossref] [PubMed]
- Mehra P, Wolford LM, Baran S, et al. Single-stage comprehensive surgical treatment of the rheumatoid arthritis temporomandibular joint patient. J Oral Maxillofac Surg 2009;67:1859-72. [Crossref] [PubMed]
- Wolford LM, Pinto LP, Cárdenas LE, et al. Outcomes of treatment with custom-made temporomandibular joint total joint prostheses and maxillomandibular counter-clockwise rotation. Proc (Bayl Univ Med Cent) 2008;21:18-24. [Crossref] [PubMed]
- Perez DE, Wolford LM, Schneiderman E, et al. Does Unilateral Temporomandibular Total Joint Reconstruction Result in Contralateral Joint Pain and Dysfunction? J Oral Maxillofac Surg 2016;74:1539-47. [Crossref] [PubMed]
- Wolford LM, Mercuri LG, Schneiderman ED, et al. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg 2015;73:952-60. [Crossref] [PubMed]
- Wolford LM, Kesterke MJ. Does Combined Temporomandibular Joint Reconstruction With Patient-Fitted Total Joint Prosthesis and Orthognathic Surgery Provide Stable Skeletal and Occlusal Outcomes in Juvenile Idiopathic Arthritis Patients? J Oral Maxillofac Surg 2022;80:138-50. [Crossref] [PubMed]
- Riolo ML, Moyers RE, McNamara JA, et al. An atlas of craniofacial growth: Cephalometric standards from the University School Growth Study, The University of Michigan. Ann Arbor, MI: University of Michigan 1974:105-6.
- Wolford LM, Karras SC, Mehra P. Considerations for orthognathic surgery during growth, part 1: mandibular deformities. Am J Orthod Dentofacial Orthop 2001;119:95-101. [Crossref] [PubMed]
- Wolford LM, Karras SC, Mehra P. Considerations for orthognathic surgery during growth, part 2: maxillary deformities. Am J Orthod Dentofacial Orthop 2001;119:102-5. [Crossref] [PubMed]
- Wolford LM, Rodrigues DB. Orthognathic considerations in the young patient and effects on facial growth. In: Preedy VR (ed). Handbook of growth and growth monitoring in health and disease. Springer, New York, 2012:1789-808.
- Wolford LM, Rodrigues DB. Temporomandibular joint (TMJ) pathologies in growing patients: Effects on facial growth and development. In: Preedy VR (ed). Handbook of growth and growth monitoring in health and disease. Springer, New York, 2012:1809-28.
- Wolford LM, Karras SC. Autologous fat transplantation around temporomandibular joint total joint prostheses: preliminary treatment outcomes. J Oral Maxillofac Surg 1997;55:245-51; discussion 251-2. [Crossref] [PubMed]
- Wolford LM, Morales-Ryan CA, Garcia-Morales P, et al. Autologous fat grafts placed around temporomandibular joint (TMJ) total joint prostheses to prevent heterotopic bone. Proc (Bayl Univ Med Cent) 2008;21:248-54. [PubMed]
- Wolford LM, Cassano DS. Autologous fat grafts around temporomandibular joint (TMJ) total joint prostheses to prevent heterotopic bone. In: Shiffman MA (ed.). Autologous fat transfer. Springer-Verlag Berlin Heidelberg 2010:361-82.
- Mercuri LG, Ali FA, Woolson R. Outcomes of total alloplastic replacement with periarticular autogenous fat grafting for management of reankylosis of the temporomandibular joint. J Oral Maxillofac Surg 2008;66:1794-803. [Crossref] [PubMed]
- Wolford L, Movahed R, Teschke M, et al. Temporomandibular Joint Ankylosis Can Be Successfully Treated With TMJ Concepts Patient-Fitted Total Joint Prosthesis and Autogenous Fat Grafts. J Oral Maxillofac Surg 2016;74:1215-27. [Crossref] [PubMed]
- Wolford L. Diagnosis and management of TMJ heterotopic bone and ankylosis. In: Bouloux GF (Editor). Complications of temporomandibular joint surgery. Switzerland: Springer International Publishing, 2017:111-33.
- Reiche-Fischel O, Wolford LM, Pitta M. Facial contour reconstruction using an autologous free fat graft: a case report with 18-year follow-up. J Oral Maxillofac Surg 2000;58:103-6. [Crossref] [PubMed]
- Henry CH, Wolford LM. Treatment outcomes for TMJ reconstruction after proplast-teflon implant failure. J Oral Maxillofac Surg 1993;51:352-8. [Crossref] [PubMed]
- Freitas R, Mehra P, Wolford LM. Autogenous versus alloplastic TMJ reconstruction in rheumatoid-induced TMJ disease. J Oral Maxillofac Surg 2002;58:43.
- Wolford LM, McPhillips A, Rodrigues D. TMJ ankylosis in children: Comparison of 3 methods of joint reconstruction. AAOMS Annual Meeting Abstract, 2009.
- Saeed N, Hensher R. Reconstruction of the TMJ autogenous compared with alloplastic. Br J Oral Maxillofac Surg 2002;40:296-9. [Crossref] [PubMed]
- Mehra P, Henry CH, Giglou KR. Temporomandibular Joint Reconstruction in Patients With Autoimmune/Connective Tissue Disease. J Oral Maxillofac Surg 2018;76:1660-4. [Crossref] [PubMed]
- Movahed R, Teschke M, Wolford LM. Protocol for concomitant temprormandibular joint custom-fitted total joint reconstruction and orthognathic surgery utilizing computer-assisted surgical simulation. J Oral Maxillofac Surg 2013;71:2123-9. [Crossref] [PubMed]
- Wolford LM. Computer-Assisted Surgical Simulation for Concomitant Temporomandibular Joint Custom-Fitted Total Joint Reconstruction and Orthognathic Surgery. Atlas Oral Maxillofac Surg Clin North Am 2016;24:55-66. [Crossref] [PubMed]
- Coleta KE, Wolford LM, Gonçalves JR, et al. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part II--airway changes and stability. Int J Oral Maxillofac Surg 2009;38:228-35. [Crossref] [PubMed]
- Mehra P, Downie M, Pita MC, et al. Pharyngeal airway space changes after counterclockwise rotation of the maxillomandibular complex. Am J Orthod Dentofacial Orthop 2001;120:154-9. [Crossref] [PubMed]
- Goncalves JR, Buschang PH, Goncalves DG, et al. Postsurgical stability of oropharyngeal airway changes following counter-clockwise maxillo-mandibular advancement surgery. J Oral Maxillofac Surg 2006;64:755-62. [Crossref] [PubMed]
- Yuen H, Rossouw PE, Wolford LM, et al. Pharyngeal Airway Space Changes After Condylar Replacement and Mandibular Advancement Surgery. J Oral Maxillofac Surg 2018;76:1165-74. [Crossref] [PubMed]
- Pinto LP, Wolford LM, Buschang PH, et al. Maxillo-mandibular counter-clockwise rotation and mandibular advancement with TMJ Concepts total joint prostheses: part III--pain and dysfunction outcomes. Int J Oral Maxillofac Surg 2009;38:326-31. [Crossref] [PubMed]
Cite this article as: Wolford LM, Kesterke MJ, Harrison CE 2nd. The efficacy of patient-fitted total joint prostheses and orthognathic surgery to reconstruct patients with congenital craniofacial deformities and temporomandibular joint malformation: a systematic review. Front Oral Maxillofac Med 2023;5:21.

