
Arthritic diseases: an indication for alloplastic temporomandibular joint replacement
Introduction
Temporomandibular joint (TMJ) arthritis
Incidence
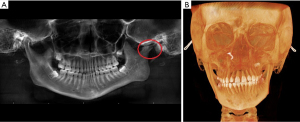
Arthritis is a collection of low- and high-inflammatory conditions that cause bony and soft tissue deterioration within an articulating joint. The terms “Arthritis” or “Degenerative joint disease” (DJD) are often used interchangeably in the literature, but DJD should ideally refer to only non-inflammatory, wear and tear related changes as noted in osteoarthritis (OA). Pain and decreased function of the joint are common sequela of such conditions. DJD can affect any joint in the body, including the TMJ. Structural and functional changes because of arthritic diseases in the TMJ can affect jaw function and cause significant impairment and distress to patients. Irrespective of the type and cause, general consequences of TMJ arthritis are inclusive but not limited to pain, malocclusion, limitation in mouth opening, masticatory insufficiency, abnormal wear of teeth, etc. Most common arthritis is OA with approximately 16% of the general population reported to have clinical symptoms of TMJ involvement. In an arthroscopy-based study by Israel et al., 68% of the joints showed arthroscopic changes consistent with DJD whereas only 3% of them were diagnosed clinically (1,2). OA is presumed to be an age-related consequence with an increase in prevalence among older patients (3,4). In most cases, surgical management of TMJ arthritis is usually indicated after failure of nonsurgical management (5). Use of total joint replacement (TJR) in TMJ arthritis is typically limited to late or end stage DJD in both low and high inflammatory arthritis, especially in patients with resultant malocclusion, retrusion of mandible, and ankylosis (Figure 1).

Types of TMJ arthritis
Low-inflammatory arthritic conditions
These conditions include OA, which starts in the articular surface of the joint, and then affects subchondral bone and joint capsule secondarily. Low-inflammatory conditions are characterized by a low leukocyte count in synovial fluid with the affected joint showing intrinsic degeneration in the articular cartilage because of functional overload, which shows up as focal degeneration on imaging (6,7). OA is considered a disease of the bone, cartilage, and supporting tissues resulting from a combination of biologic and mechanical processes that decrease the turnover of subchondral bone and articular cartilage resulting in degeneration of cartilage with subsequent osseous erosion, sclerosis, and osteophyte formation seen at the margins (5,7,8). Most patients with early-stage disease can be successfully managed non-surgically and/or with minimally invasive procedures (6,9-11). Idiopathic condylar resorption (ICR) is also a low-inflammatory condition but of unknown etiology. A detailed discussion of ICR can be found in another paper in this series entitled “The role of alloplastic temporomandibular joint (TMJ) replacement in the management of condylar resorption—a narrative review of the literature” (12).
High-inflammatory arthritic conditions
These systemic disorders are well known with examples such as rheumatoid arthritis (RA), ankylosing spondylitis (AS), psoriatic arthritis (PA) and juvenile idiopathic arthritis (JIA) and metabolic arthritis (MA) (such as gout, pseudogout etc.) (10). The TMJs could potentially be affected by any of these conditions, and to varying incidence and severity (13). These inflammatory diseases can not only cause pain, dysfunction due to limited movement and muscle spasm, but also progression of the disease in skeletally immature patients leads to joint destruction resulting in mandibular growth disturbances, malocclusion, facial deformity and in some cases TMJ ankylosis (13-15). The diagnosis of TMJ involvement in high-inflammatory/systemic arthritic diseases is established by correlating the patients’ history, clinical exam findings, imaging characteristics, and laboratory testing results (rheumatoid factor, erythrocyte sedimentation rate, C-reactive protein, antinuclear antibody, anti-cyclic citrullinated peptide etc.).
The most common in this group is RA with its prevalence among general population ranging from 0.5–1% (16). The incidence of TMJ involvement among RA cases varies significantly (5–86%) with bilateral TMJ involvement in about 34–75% of cases (13-17). TMJ involvement in PA and AS, varies around 35% to 50% and 11% to 35% respectively, with usually less severe symptoms (18,19). JIA is the most common pediatric rheumatologic condition affecting the TMJs with more than 40% of them showing TMJ involvement. The overall incidence varies according to the subtype from 17% to 87%, with bilateral disease seen in 53% to 83% of affected patients (20,21).
RA
RA is characterized by an infiltrating, inflammatory synovial tissue mass formed secondary to hyperplasia of type A fibroblast-like synovial cells which leads to damage in the cartilage, bone, and tendons. This happens because of infiltration with monocyte/macrophage and lymphocyte etc. (22). TMJ is one of the last joints in the body affected by RA. A recent study by Ozcan et al. reported clinical involvement of the TMJ in about 65% of patients and radiologic evidence seen in 76% of patients diagnosed with RA (23). Patients can present with dull aching pain associated with jaw function, edema of the joint, and limited range of motion of the mandible. Anterior open bites can be seen in bilateral cases. Morning stiffness or stiffness at rest can commonly last longer than an hour. Radiographic presentation can range from flattening of the condyle to severe deformity (24). Ankylosis can be unilateral or bilateral but is an uncommon finding presenting in late stages (25,26). Juvenile onset commonly leads to facial deformities which when unilateral may seem to be consistent with contralateral condylar hyperplasia including occlusal canting and unilateral loss of ramal height. (Figure 2A,2B). In severe bilateral cases, loss of condyle-ramus height leads to retrognathia and anterior open bite with resultant narrowing of posterior airway space and obstruction causing sleep apnea (27,28). Patients with RA more commonly show radiographic changes in the TMJ than the ones with PA or AS (28-30). Common radiographic signs of RA such as flattening of the head of the condyle/articular eminence, erosion of the cortex, subchondral cysts, sclerosis, and decrease in joint space are non-specific (29,30).
PA
PA in TMJ may initially present as joint noises, pain, morning stiffness, tenderness in muscle, crepitus while advanced cases can show limited movement secondary to fibrosis and crepitus associated with structural changes (31-33). Patients with PA have a higher incidence of TMJ involvement and increased severity as opposed to patients without arthritic component (31). Increased severity of symptoms, prolonged duration, higher number of joints involved in PA were found to be significant risk factors for TMJ involvement while difference in gender was not (32). Non-specific radiographic signs, clinical symptoms and laboratory findings with lack of correlation to severity of skin symptoms can make diagnosis of PA challenging. The criteria for diagnosis of psoriatic arthropathy in the TMJ includes prior diagnosis of psoriasis, erosive poly-arthropathy, and negative serology testing for rheumatoid factor (34,35). Although no correlation exists between severity of skin symptoms and arthropathy, examination of the skin, nails, scalp and umbilicus can help when PA of TMJ is suspected in an undiagnosed patient (36). Clinical signs such as nail bed separation (onycholysis) and pitting can be seen in about 85% of patients with PA. Conjunctivitis, uveitis and iritis can be seen. Psoriatic lesions can sometimes develop in skin areas subject to trauma, this is defined as Koebner phenomenon (37). Structural changes such as condylar erosion/flattening, osteophyte formation, decreased joint space, subchondral sclerosis, and signs like joint collapse, shortening of ramus height, and ankylosis are encountered in late-stage disease (36).
AS
AS is a seronegative progressive inflammatory condition of the spine. It involves synovial proliferation which causes cartilage loss and in-growth of granulation tissue into the bone (38,39). AS commonly occurs in the sacroiliac joint, and TMJ involvement has been reported to be in up to 22% of affected patients (39). Most patients are asymptomatic and clinical symptoms of the disease are non-specific. Clinical signs of AS in the TMJ may include joint noises, tenderness over the muscles of mastication, masseteric hypertrophy, and limited mouth opening (39-42). Although clinical signs and symptoms are found less often and are less severe compared to rheumatoid or PA, resorption of bone and ankylosis have been reported in advanced cases of AS (42,43).
JIA
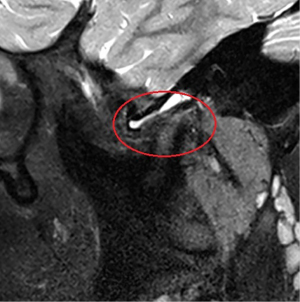
JIA previously known as juvenile rheumatoid arthritis (JRA) is a broad group of heterogenous arthritic diseases of an unknown cause. JIA is one of the most common pediatric rheumatologic conditions in the USA. JIA is a systemic disease that causes synovial inflammation and subsequent loss of soft and hard tissues of the joints. Greater than 40% of patients diagnosed with JIA can show involvement of the TMJ (20). JIA and ICR are two different entities and should be differentiated to avoid confusion. ICR is limited to the TMJ and presents without synovitis and inflammation of the joints (20). Early detection and medical management of JIA may avoid the need for invasive TMJ TJR or orthognathic surgery later. When the disease is aggressive, delay in diagnosis and/or treatment can lead to joint erosions, effusions, decrease in joint space. Active synovitis shows as an enhancement of the intra-articular tissues on magnetic resonance imaging (MRI) with gadolinium contrast. Although laboratory studies may provide additional information to aid in diagnosing JIA, normal laboratory values do not automatically correlate to a negative JIA diagnosis.
Clinical/radiographic presentation from TMJ arthritis
Patients with TMJ arthritis can present a wide array of clinical symptoms ranging from pain, dysfunction, and difficulty with mastication to complete inability to open the mouth. Arthritic conditions affecting the TMJ can create some non-specific as well as unique radiographic changes within the joint anatomy. Standard imaging for monitoring bone architecture includes computerized tomography (CT) scans [cone beam computed tomography (CBCT)/medical grade] while MRI scans are considered the gold standard for soft tissue imaging including the disc and synovial tissues. In systemic inflammatory arthritic conditions such as JIA, MRI with gadolinium contrast may help improve visualization of the active inflammation in the joint (Figure 3).
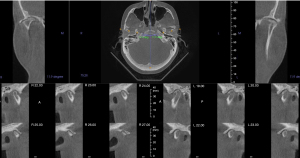
Most arthritic conditions present with pain in the affected joints. Pain in the TMJ region can arise from soft tissues of the joint, subchondral bone and/or the muscles of mastication in reflex contraction to protect the joint from further damage (7). This reflex muscular contraction mechanism is self-preserving for the pathologically affected joint and limits its motion. Other notable signs and symptoms of TMJ arthritis are loss of joint anatomy or instability, malocclusion/facial deformity from loss of ramal height which results in apertognathia or late stage ankylosis of the TMJ (10) (Figure 4).

Indications for TMJR in patients with TMJ arthritis
When there is significant erosion or destruction of the joint secondary to arthritic diseases, the most predictable treatment for the degenerative, ankylotic, or collapsed joint is total TMJ replacement or reconstruction. Collapse of the joint can present with signs and symptoms such as malocclusion, decreased jaw function, masticatory dysfunction, trismus, muscle spasms and pain. Though improvement of function and reduction of pain are often the main indications in TJR surgery for advanced and refractory TMJ arthritis patients, worsening or persistent malocclusions can also be an indication for alloplastic total joint reconstruction as it provides for excellent long-term skeletal stability as opposed to traditional mandibular osteotomies for advancement and rotation (44). Use of autogenous grafts such as costochondral grafts has become a rarity due to their multiple drawbacks, which include a higher risk of re-ankylosis, donor site morbidity, need for postoperative maxillomandibular fixation, and the unknown effect of the systemic inflammation on autogenous bone (45,46). Use of costochondral grafts is largely limited to pediatric patients where some jaw growth potential may be desired. Almost universally, alloplastic TJR is now considered the standard and most efficient option for TMJ reconstruction in arthritis patients (47).
Alloplastic total joint reconstruction of the TMJ was first developed in the 1990s and has come a long way over the past 3 decades (48). Currently, there are two aalloplastic total joint reconstruction prostheses that are FDA approved in the United States. These are the patient-fitted prosthesis (TMJ Concepts/Stryker, Ventura, CA, USA) and the stock prosthesis (Zimmer Biomet, Jacksonville, FL, USA). There are over two dozen alloplastic total joint systems around the world, but most do not have a long-term record and have varying designs, composition, duration of preclinical testing and composition (49).
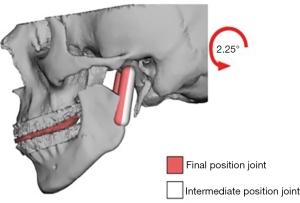
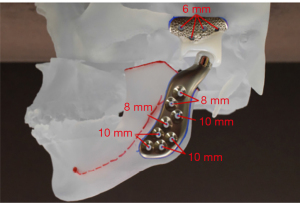
TMJ Concepts patient-fitted prostheses are milled based on computer-aided design and manufacture (CAD-CAM) skull models from a three-dimensional CT or CBCT) (Figure 5). If patient requires a combined orthognathic-TMJ replacement operation, CBCT data is first used for virtual surgical planning to determine final maxillary/mandibular position and then the CBCT data is then transferred to the prosthesis manufacturer (Figure 6). The long-term follow up studies in general show more than 90% success rates with over 20 years of follow-up reported significant improvement in mouth opening, and diet, and decrease in pain (50). The prosthesis is composed of an ultra-high molecular weight polyethylene fossa with a Titanium alloy mesh while the ramus segment is made of Titanium alloy with CO-Cr condyle head (Figure 7). The prosthesis components are fixated to the lateral surface of the zygomatic arch/fossa and ramus of the mandible. The head of the condyle component can be made with hardened titanium-only option in patients who are allergic to the usual cobalt-chromium alloy or other component metals. The Zimmer Biomet prosthesis is available in stock option only in the United States, but the custom version is available outside the US. The Zimmer Biomet prosthesis also has a similar long-term follow-up record with proven efficacy (51).
The total joint reconstruction of TMJ in patients with inflammatory arthritic conditions such as RA, PA, AS, MA can be more complex due to deformed anatomy, ingrowth of inflamed tissue into the joint and TMJ ankylosis. The systemic disease status, immunosuppression, and their general functional limitations can also affect early post-operative course and long-term outcomes including the rate of prosthetic joint infections (PJI). In a study done by O’Connor et al. the outcomes of TMJR in patients with high-inflammatory conditions were comparable to TMJR in patients without despite the above referenced challenges (44). In case of patients receiving unilateral TMJR, current literature evidence does not support performing contralateral TMJR unless showing similar indications for TMJR (44,47,49).
Outcomes of TMJR in TMJ arthritis
Replacement of the TMJ helps correct the malocclusion and dentofacial deformity, while improving mouth opening and diet tolerance (44). Outcomes of a prospective study by O’Connor et al. on alloplastic reconstruction of the TMJ in patients with systemic inflammatory arthritic conditions showed that at one year, patients who underwent TMJ TJR (including 4 PA, 1 AS, and 9 with RA) had improvement of up to 90% in pain and dietary scores, and about 11 mm of mean increase in mouth opening. Pain scores [visual analogue scale (VAS), 1–100], dietary function and mouth opening were measured at pre-operative condition, at 6 weeks, 6 months, one year, and beyond post-operatively. Forty-six joints were reconstructed in 26 patients, majority were women. The common indications were RA (n=17) and PA (n=7). At 1-year post-operation, mean reduction in pain scores were from 55 to 2 on the left side and from 62 to 2 on the right (P<0.001). Dietary scores improved from a mean of 48 to 95, while mean of mouth opening measurements improved from 23 to 35 mm (P<0.001). Long-term follow up showed stability of the outcomes (44). Another retrospective study by Sarlabous et al. which looked at outcomes of alloplastic total joint reconstruction of TMJ in patients with systemic inflammatory arthritic conditions showed, RA to be the most common diagnosis in their subjects followed by JIA, AS, PA, lupus, and mixed connective tissue disorder. The pain scores in this study showed a mean decrease from 6.8 at pre-surgery to 1.3 (P<0.001) at the longest follow up. The mouth opening improved from a mean of 22.1 mm before surgery to 34.3 mm (P<0.001) at last follow-up (13).
Alternative surgical/non-surgical management
Initial management of TMJ arthritis includes non-surgical measures such as non-steroidal anti-inflammatory drugs (NSAIDs), diet modification, moist heat, jaw relaxation, physical therapy, and oral appliances (52). Approximately 80% of patients may report significant improvement in their symptomatology with these non-surgical methods themselves (52). Physical therapy can help manage limited mouth opening while NSAIDs are indicated for pain secondary to inflammation (50,53). No specific design of an oral appliance has been proven to be more advantageous than the others; hence, a simple full coverage upper/lower appliance can provide benefits without risk of occlusal changes (54). A diagnostic local anesthetic injection into the joint space can help localize, confirm, and temporarily subside the intra-articular pain. Arthroscopy may provide additional diagnostic information besides having some therapeutic benefit.
Persistent synovitis up to 6 weeks after arthroscopy or arthrocentesis may improve from intra-articular steroid injections. Intra-articular steroid injections are not routinely performed but shown to be of value in patients with acute synovitis in high-inflammatory arthritic conditions of the joint. These are generally limited to 1–2 injections over 6–12 months. Some studies show that less than 10% of these patients may require arthroscopic intervention, and another 10% may require a subsequent open TMJ surgery (53,55). Outcomes are generally considered to be less favorable among patients with high inflammatory arthritis, but there have been no large-scale studies to provide definitive evidence. Arthroscopy can be difficult to perform in patients with ankylosing conditions due to lack of joint space. Historically speaking, TMJ disorders that were unresponsive or less than optimally responsive to nonsurgical or minimally invasive procedures have been managed with different types of open surgical operations. Clinicians must be cognizant of the fact that indiscriminate use of surgical procedures can possibly result in development of secondary DJD and/or dysesthesia that is refractory to analgesic treatments. Synovectomy to manage or treat rheumatologic conditions is complex and difficult procedure to perform in the TMJ given the proximity of vital structures on the medial side of the joint (56). Discectomy is considered in TMJs with grossly deformed and/or immobile discs with/without perforation that are deemed non-salvageable or beyond repair. Discectomy may be supplemented with interpositional grafts, but current evidence shows no additional benefit as opposed to discectomy alone. Without the interpositional graft, the joint is presumed to remodel while forming a “pseudo disc” or “neo disc” from the fibrous tissue formed in place of the disc. In a functional TMJ, repeating arthroscopy or arthrocentesis with cautious use of intraarticular medications has been shown to be successful (27).
Conclusions
Patients with a low or high inflammatory arthritis affecting the TMJ may require TMJ replacement. Given the nature of high-inflammatory arthritis with resultant bony erosion, these patients may have a lower threshold for a TMJR when compared to patients with low-inflammatory conditions. Although knowledge about the high inflammatory arthritic conditions shows higher risk for complications, recent studies support a positive functional result. Current evidence shows that TMJR significantly improves function and quality of life in patients with arthritic conditions. Within currently available options, in our opinion, a patient-fitted prosthesis would be preferred, although stock prostheses also provide similar outcomes.
Through this paper we focused on fundamentals of alloplastic TMJ reconstruction as an indication for inflammatory disease of the TMJ. Pertinent and contemporary literature was reviewed while highlighting currently accepted treatment guidelines. Alloplastic total joint reconstruction for TMJ has several benefits over autogenous options and hence should be considered as first choice when joint replacement is warranted in patients with TMJ arthritis.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Louis Mercuri) for the series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” published in Frontiers of Oral and Maxillofacial Medicine. The article has undergone external peer review.
Peer Review File: Available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-29/prf
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.com/article/view/10.21037/fomm-22-29/coif). The series “Indications for Alloplastic TMJ Replacement in Maxillofacial Surgery—an evidence-based review of the literature” was commissioned by the editorial office without any funding or sponsorship. SKR was an immediate past president for Virginia Society of Oral and Maxillofacial Surgeons, Virginia, USA, and SKR is a Member Committee on Research Planning and Technology Assessment at American Association of Oral and Maxillofacial surgeons (AAOMS). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for publication.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mejersjo C. Therapeutic and prognostic considerations in TMJ osteoarthrosis: a literature review and a long-term study in 11 subjects. Cranio 1987;5:69-78. [Crossref] [PubMed]
- Israel HA, Saed-Nejad F, Ratcliffe A. Early diagnosis of osteoarthrosis of the temporomandibular joint: correlation between arthroscopic diagnosis and keratan sulfate levels in the synovial fluid. J Oral Maxillofac Surg 1991;49:708-11; discussion 712. [Crossref] [PubMed]
- Garstang SV, Stitik TP. Osteoarthritis: epidemiology, risk factors, and pathophysiology. Am J Phys Med Rehabil 2006;85:S2-11; quiz S12-4. [Crossref] [PubMed]
- Goldring MB, Goldring SR. Osteoarthritis. J Cell Physiol 2007;213:626-34. [Crossref] [PubMed]
- Teruel A, Broussard JS, Clark GT. Temporomandibular Joint Arthritis: Implications, Diagnosis, and Management. In: Clark GT, Dionne RA. editors. Orofacial Pain. West Sussex, UK: John Wiley & Sons, Inc., 2012:311-25.
- Mercuri LG. Osteoarthritis, osteoarthrosis, and idiopathic condylar resorption. Oral Maxillofac Surg Clin North Am 2008;20:169-83. v-vi. [Crossref] [PubMed]
- Sah RL, Chen AC, Chen SS, et al. Articular cartilage repair. In: Koopman W. editor. Arthritis and Allied Conditions—A Textbook of Rheumatology. Philadelphia: Lippincott Williams & Wilkins, 2001:112.
- Felson DT, Lawrence RC, Dieppe PA, et al. Osteoarthritis: new insights. Part 2. The disease and its risk factors. Ann Intern Med 2000;133:726-37. [Crossref] [PubMed]
- Mercuri LG. Surgical management of TMJ arthritis. In: Laskin DM, Greene CS, Hylander WL. editors. TMDs, an evidence-based approach to diagnosis and treatment. Chicago: Quintessence, 2006:455-68.
- Mercuri LG, Abramowicz S. Arthritic Conditions Affecting the Temporomandibular Joint. In: Farah C, Balasubramaniam R, McCullough M. editors. Contemporary Oral Medicine. Springer International Publishing, 2019:1919-54.
- Laskin DM. Temporomandibular Joint Pain. In: Firestein GS, Budd RC, Gabriel SE, et al. editors. Kelley and Firestein's Textbook of Rheumatology (Tenth Edition). Elsevier, 2017:756-67.
- Mercuri LG. The role of alloplastic temporomandibular joint (TMJ) replacement in the management of condylar resorption—a narrative review of the literature. Front Oral Maxillofac Med 2023;5:34.
- Sarlabous M, El-Rabbany M, Caminiti M, et al. Alloplastic Temporomandibular Joint Replacement in Patients With Systemic Inflammatory Arthritis and Connective Tissue Disorders. J Oral Maxillofac Surg 2021;79:2240-6. [Crossref] [PubMed]
- Ruparelia PB, Shah DS, Ruparelia K, et al. Bilateral TMJ Involvement in Rheumatoid Arthritis. Case Rep Dent 2014;2014:262430. [Crossref] [PubMed]
- Bessa-Nogueira RV, Vasconcelos BC, Duarte AP, et al. Targeted assessment of the temporomandibular joint in patients with rheumatoid arthritis. J Oral Maxillofac Surg 2008;66:1804-11. [Crossref] [PubMed]
- Cordeiro PC, Guimaraes JP, de Souza VA, et al. Temporomandibular joint involvement in rheumatoid arthritis patients: association between clinical and tomographic data. Acta Odontol Latinoam 2016;29:123-9. [PubMed]
- Aliko A, Ciancaglini R, Alushi A, et al. Temporomandibular joint involvement in rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. Int J Oral Maxillofac Surg 2011;40:704-9. [Crossref] [PubMed]
- de Oliveira-Neto PJ, Marchiori EC, de Almeida Lopes MC, et al. Bilateral alloplastic prostheses for temporomandibular joint reconstruction in a patient with ankylosing spondylitis. Craniomaxillofac Trauma Reconstr 2014;7:149-53. [Crossref] [PubMed]
- Arora P, Amarnath J, Ravindra SV, et al. Temporomandibular joint involvement in ankylosing spondylitis. BMJ Case Rep 2013; [Crossref] [PubMed]
- Abramowicz S, Kim S, Prahalad S, et al. Juvenile arthritis: current concepts in terminology, etiopathogenesis, diagnosis, and management. Int J Oral Maxillofac Surg 2016;45:801-12. [Crossref] [PubMed]
- El Assar de la Fuente S, Angenete O, Jellestad S, et al. Juvenile idiopathic arthritis and the temporomandibular joint: A comprehensive review. J Craniomaxillofac Surg 2016;44:597-607. [Crossref] [PubMed]
- Jasin H. Mechanisms of tissue damage in rheumatoid arthritis. In: Koopman W. editor. Arthritis and Allied Conditions—A Textbook of Rheumatology. Philadelphia: Lippincott Williams & Wilkins, 2001:57.
- Ozcan I, Ozcan KM, Keskin D, et al. Temporomandibular joint involvement in rheumatoid arthritis: correlation of clinical, laboratory and magnetic resonance imaging findings. B-ENT 2008;4:19-24. [PubMed]
- Helenius LM, Hallikainen D, Helenius I, et al. Clinical and radiographic findings of the temporomandibular joint in patients with various rheumatic diseases. A case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:455-63. [Crossref] [PubMed]
- Lurie R, Fisher JT, Lownie JF. Temporomandibular joint ankylosis in rheumatoid arthritis. A case report. S Afr Med J 1988;73:57-8. [PubMed]
- Kobayashi R, Utsunomiya T, Yamamoto H, et al. Ankylosis of the temporomandibular joint caused by rheumatoid arthritis: a pathological study and review. J Oral Sci 2001;43:97-101. [Crossref] [PubMed]
- Sidebottom AJ, Salha R. Management of the temporomandibular joint in rheumatoid disorders. Br J Oral Maxillofac Surg 2013;51:191-8. [Crossref] [PubMed]
- Redlund-Johnell I. Upper airway obstruction in patients with rheumatoid arthritis and temporomandibular joint destruction. Scand J Rheumatol 1988;17:273-9. [Crossref] [PubMed]
- Wenneberg B, Könönen M, Kallenberg A. Radiographic changes in the temporomandibular joint of patients with rheumatoid arthritis, psoriatic, arthritis, and ankylosing spondylitis. J Craniomandib Disord 1990;4:35-9. [PubMed]
- Ardic F, Gokharman D, Atsu S, et al. The comprehensive evaluation of temporomandibular disorders seen in rheumatoid arthritis. Aust Dent J 2006;51:23-8. [Crossref] [PubMed]
- Dervis E, Dervis E. The prevalence of temporomandibular disorders in patients with psoriasis with or without psoriatic arthritis. J Oral Rehabil 2005;32:786-93. [Crossref] [PubMed]
- Könönen M. Subjective symptoms from the stomatognathic system in patients with psoriatic arthritis. Acta Odontol Scand 1986;44:377-83. [Crossref] [PubMed]
- Könönen M. Craniomandibular disorders in psoriasis. Community Dent Oral Epidemiol 1987;15:108-12. [Crossref] [PubMed]
- Boyle JA, Buchanan WW. Clinical rheumatology. Oxford: Blackwell Scientific, 1971:304-17.
- Wilson AW, Brown JS, Ord RA. Psoriatic arthropathy of the temporomandibular joint. Oral Surg Oral Med Oral Pathol 1990;70:555-8. [Crossref] [PubMed]
- Lundberg M, Ericson S. Changes in the temporomandibular joint in psoriasis arthropathica. Acta Derm Venereol 1967;47:354-8. [PubMed]
- Baetz K, Klineberg I. Psoriatic arthritis of the temporomandibular joint. Case report. Aust Dent J 1986;31:335-9. [Crossref] [PubMed]
- Kumar PJ, Clark ML. editors. Clinical medicine. 7th ed. Philadelphia: Saunders Elsevier, 2009.
- Locher MC, Felder M, Sailer HF. Involvement of the temporomandibular joints in ankylosing spondylitis (Bechterew's disease). J Craniomaxillofac Surg 1996;24:205-13. [Crossref] [PubMed]
- Wilkinson M, Bywaters EG. Clinical features and course of ankylosing spondylitis; as seen in a follow-up of 222 hospital referred cases. Ann Rheum Dis 1958;17:209-28. [Crossref] [PubMed]
- Manemi RV, Fasanmade A, Revington PJ. Bilateral ankylosis of the jaw treated with total alloplastic replacement using the TMJ concepts system in a patient with ankylosing spondylitis. Br J Oral Maxillofac Surg 2009;47:159-61. [Crossref] [PubMed]
- Könönen M, Wenneberg B, Kallenberg A. Craniomandibular disorders in rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis. A clinical study. Acta Odontol Scand 1992;50:281-7. [Crossref] [PubMed]
- Miles DA, Kaugars GA. Psoriatic involvement of the temporomandibular joint. Literature review and report of two cases. Oral Surg Oral Med Oral Pathol 1991;71:770-4. [Crossref] [PubMed]
- O’Connor R, Saleem S, Sidebottom A. Prospective outcome analysis of total temporomandibular joint replacement using the TMJ concepts system in patients with rheumatological diseases. Brit J Oral Max Surg 2015;53:e121. [Crossref]
- Hawkins A, Mercuri LG, Miloro M. Are Rib Grafts Still Used for Temporomandibular Joint Reconstruction? J Oral Maxillofac Surg 2020;78:195-202. [Crossref] [PubMed]
- Mercuri LG. Costochondral Graft Versus Total Alloplastic Joint for Temporomandibular Joint Reconstruction. Oral Maxillofac Surg Clin North Am 2018;30:335-42. [Crossref] [PubMed]
- Saeed NR, McLeod NM, Hensher R. Temporomandibular joint replacement in rheumatoid-induced disease. Br J Oral Maxillofac Surg 2001;39:71-5. [Crossref] [PubMed]
- Mercuri LG. editor. Temporomandibular Joint Total Joint Replacement – TMJ TJR – A Comprehensive Reference for Researchers, Material Scientists and Surgeons. New York: Springer International Publishing, 2016.
- Elledge R, Mercuri LG, Attard A, et al. Review of emerging temporomandibular joint total joint replacement systems. Br J Oral Maxillofac Surg 2019;57:722-8. [Crossref] [PubMed]
- Wolford LM, Mercuri LG, Schneiderman ED, et al. Twenty-year follow-up study on a patient-fitted temporomandibular joint prosthesis: the Techmedica/TMJ Concepts device. J Oral Maxillofac Surg 2015;73:952-60. [Crossref] [PubMed]
- Leandro LF, Ono HY, Loureiro CC, et al. A ten-year experience and follow-up of three hundred patients fitted with the Biomet/Lorenz Microfixation TMJ replacement system. Int J Oral Maxillofac Surg 2013;42:1007-13. [Crossref] [PubMed]
- Moore RA, Tramèr MR, Carroll D, et al. Quantitative systematic review of topically applied non-steroidal anti-inflammatory drugs. BMJ 1998;316:333-8. [Crossref] [PubMed]
- Lin J, Zhang W, Jones A, et al. Efficacy of topical non-steroidal anti-inflammatory drugs in the treatment of osteoarthritis: meta-analysis of randomised controlled trials. BMJ 2004;329:324. [Crossref] [PubMed]
- Al-Ani MZ, Gray RJ, Davies SJ, et al. Anterior repositioning splint for temporomandibular joint disc displacement (protocol). Cochrane Collaboration. The Cochrane Library 2009;(1). Available online: http://www.thcochranelibrary.com
- Brennan PA, Ilankovan V. Arthrocentesis for temporomandibular joint pain dysfunction syndrome. J Oral Maxillofac Surg 2006;64:949-51. [Crossref] [PubMed]
- Sidebottom AJ. Current thinking in temporomandibular joint management. Br J Oral Maxillofac Surg 2009;47:91-4. [Crossref] [PubMed]
Cite this article as: Renapurkar SK, Mehra P. Arthritic diseases: an indication for alloplastic temporomandibular joint replacement. Front Oral Maxillofac Med 2023;5:37.

