The influence of crown-to-implant ratio on marginal bone loss: a narrative review
Introduction
Dental implants are considered nowadays a reliable solution to replace teeth. High implants and prosthesis survival rates (above 98% after 5 years) were achieved (1,2). To consider successful an implant therapy the criteria at implant level are: absence of pain, bone loss at 1st year <1.5 mm, annual bone loss <0.2 mm thereafter, no radiolucency, no mobility, no infection (3). Therefore, marginal bone loss (MBL) represents a favourable factor for long-term implant stability (4). Unfavourable crown-to-implant ratio (C/I-R), occlusal overload, occlusal table width, off-axis loading and cantilevers are factors that play a role in the failure of prosthetic implant therapy (5-7). The influence of cantilever (8), occlusal overload (9), and off-axis loading in prosthetic complications are largely demonstrated.
However, the role of C/I-R on MBL is still unclear. C/I-R is the application in implantology of the prosthodontics parameter of crown-to-root ratio. Ideally, the ratio between the crown and the root should be 1:2, and a minimum of 1:1 for a tooth abutment is recommended. To avoid unfavourable C/I-R, these prosthetic concepts have been used in implant dentistry. C/I-R is calculated as the ratio between the crown and implant lengths. We can distinguish two different C/I-R:
- Anatomical ratio is the ratio between the distance from the apex to the shoulder of the implant, and the distance from the shoulder of the implant to the end of the crown;
- Clinical ratio is the ratio between the distance from the apex to the bone level, and the distance from the bone level to the end of the crown.
In literature there are evidences that attest both the presence (10) and the absence (11,12) of a relationship between MBL and C/I-R, and one studies even deducted that high CI might provide a protective effect on bone loss (13). In addition, the introduction of short implant, to avoid bone augmentation procedure, lead to C/I-R higher and higher. A security threshold should be investigated to avoid biological complication and to guarantee the success of the therapy. The aim of this study is to elucidate about the role of C/I-R on MBL. We present the following article in accordance with the Narrative Review reporting checklist (available as http://dx.doi.org/10.21037/fomm-20-57).
Methods
The articles were identified through MEDLINE database (via PubMed) combined the key words: “crown-implant ratio”, “marginal bone loss”, “alveolar bone loss”, “short implants”. The search was supplemented checking references of the relevant review articles. The studies had to meet the following requirement:
- At least 1 year follow-up;
- Mean C-I/R should be reported;
- Outcome measures should include at least bone changes;
- Publication must be reporting in the English.
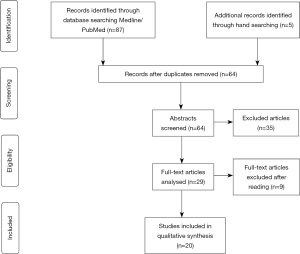
The selection path of the articles is shown in Figure 1.
Discussion/summary
The primary selection identified 87 studies for the MEDLINE search. Checking of relevant reviews revealed five additional articles that met the inclusion criteria. After having removed duplicates and analysed titles and abstracts, 58 studies were excluded because they did not meet the inclusion criteria. The remaining 29 papers were evaluated by full-text analysis. Nine articles were finally excluded after full-text reading due to lack of information as marginal bone changes and C/I-R measurement. Characteristics of the selected studies are shown in Tables 1 and 2. Anitua et al. (14) in a retrospective study analysed 45 implants with a mean C/I-R of 2.4. The mean MBL reported was 1.01 mm for mesial bone, 0.89 mm for distal bone. Birdi et al. (15) studied 309 implants in a retrospective study. The mean C/I-R reported was 2.0 and the MBL was 0.2 mm. Blanes et al. (16) in a perspective study analyzed 109 implants. The mean C/I-R was 1.77. MBL was calculated for three different groups: group A (C/I-R 0–0.99): 0.35 mm, group B (C/I-R 1–1.99): 0.03 mm, group C (C/I-R >2): 0.02 mm. Di Fiore et al. (17) studied 108 implants retrospectively with a mean C/I-R of 2.21 mm. The mean MBL reported was 1.42 mm. Guljé et al. (18) analyzed 47 implants in a perspective study. The mean C/I-R was 2.14 with a MBL reported of 0.13 mm. Hadzik et al. (19) studied perspectively 30 implants with an anatomical ratio of 1.69. MBL reported was 0.34 mm. Hingsammer et al. (20) in a perspective study analysed 76 implants. The mean C/I-R was 1.70 with a MBL of 0.71 mm. Lee et al. (21) studied retrospectively 175 implants with a mean C/I-R of 1.06, MBL reported was 0.93 mm. Malchiodi et al. (22) analyzed 280 implants in a perspective study. In the study was reported both the anatomical and the clinical ratio, that was respectively 1.84 and 2.08. The MBL calculated was 0.48 mm. Mangano et al. (23) studied 68 implants perspectively. The mean C/I-R was 1.70. After 5 years of loading, a mean MBL of 0.38 and 0.48 was reported in the C/I <2 and C/I >2 groups, respectively. Naenni et al. (24) analyzed 96 implants in a perspective cohort study. The 6-mm and the 10-mm had a mean C/I-R of 1.75 and 1.04, respectively. The mean MBL calculated was 0.29 mm for the 6-mm group, and 0.15 mm for the 10-mm group. Nunes et al. (25) studied 118 implants retrospectively. The mean C/I-R was 2.53 and the MBL calculated was 0.67 mm. Pieri et al. (26) in a perspective study analyzed 61 implants with a mean C/I-R of 1.94 mm. The MBL calculated at 2 years was 0.60 mm. Ramaglia et al. (27) studied perspectively 78 implants with a mean C/I-R of 1.08. MBL at 5-year was calculated separately for the C/I-R <1 and C/I-R >1 group and was 0.653 and 0.287 mm respectively. Rossi et al. (28) in a perspective study confronted two groups of 30 implants each. The mean C/I-R for test and control group was 1.55 and 0.97 respectively. After 5-year loading MBL calculated was 0.14 mm for test group and 0.18 mm for control group. Schneider et al. (29) in a retrospective study analyzed 100 implants. In the study was reported both the anatomical and the clinical C/I-R of 1.04 and 1.48 respectively. The MBL calculated was 0.008 mm. Sharmann et al. (30) analyzed perspectively two different groups of 47 implants each. The mean C/I-R reported was 0.86 for the control group and 1.48 for the test group. The mean MBL calculated after 3 years were 0.19 and 0.33 for the test and control groups respectively. Urdaneta et al. (31) in a retrospective study analyzed 326 implants with a mean C/I-R of 1.6. The mean MBL found was 0.33 mm. Villarinho et al. (32) analyzed 46 implants perspectively. The mean C/I-R reported was 1.6 with a MBL of 0.3 mm. Zadeh et al. (33) analyzed perspectively for 3 years 209 implants divided in two groups. The C/I-R was 1.78 for the test group and 0.93 for the control group. The analysis of MBL revealed that the test group gained 0.04 mm while the control group losed 0.02 mm. Overall, the highest follow-up reported was 16 years for the retrospective studies and 5 years for the prospective studies. The highest C/I-R reported was 2.5.
Table 1
| Article | Years of publication | C/I-R considered | Mean C/I-R | Mean CHS | Survival rate | Marginal bone changes |
|---|---|---|---|---|---|---|
| Anitua et al. | 2014 | Clinical | 2.4 (1.5 to 3.69) | 17.05±3.05 mm (11.2 to 25.4 mm) | 100% | Mesial bone loss 1.01±0.68 mm (range 0 to 3.49 mm); distal bone loss 0.89±0.7 mm (range 0 to 3.86 mm) |
| Birdi et al. | 2010 | Clinical | 2.0 ±0.4 (0.92–3.2) | 13.3±2.6 mm (6.2–21.7) | – | Mesial: −0.2±0.7 mm; distal: −0.2±0.9 mm |
| Blanes et al. | 2007 | Clinical | 1.77±0.56 mm | Anatomical crown length: 9.57±2.6 mm; clinical crown length: 13.57±2.73 mm | Group ratio >2 mm: 94.1% | Group A (C/I-R: 0–0.99): −0.35±0.27 mm; Group B (C/I-R: 1–1.99): −0.03±0.15 mm; Group C (C/I-R >2): −0.02±0.26 mm |
| Di Fiore et al. | 2019 | Clinical | 2.21±0.31 mm | 10.86±0.99 mm | – | −1.42±0.38 mm |
| Guljé et al. | 2016 | Clinical | 2.14±0.42 (1.16 to 3.23) | – | 100% | −0.13±0.36 mm |
| Hadzik et al. | 2018 | Anatomical | 1.69 | – | – | −0.34±0.24 mm |
| Hingsammer et al. | 2017 | Clinical | 1.70 (SD: 0.48) | 9.9 mm (SD: 1.24 mm; range: 8.1–12.4 mm) | 97.3% | −0.71 mm (SD: 0.74 mm) |
| Lee et al. | 2012 | Clinical | 1.06±0.42 | – | – | −0.93±0.15 mm (range, 0.05 to 1.89 mm) |
| Malchiodi et al. | 2014 | Clinical and anatomical | Anatomical: 1.84±0.65 (range: 0.86–4.28); Clinical: 2.08±0.80 (range: 0.95–4.80) | – | 98.1% | −0.48±0.29 mm |
| Mangano et al. | 2016 | Clinical | 1.70 (0.25; median 1.72; range 1.40–2.25; 95% CI: 1.65–1.75). | – | 97% | C/I-R <2: 0.38 mm; C/I-R >2: 0.48 mm |
| Naenni et al. | 2018 | Anatomical | 6-mm group: 1.75 (IQR, 1.50 to 1.90); 10-mm group: 1.04 (IQR, 0.95 to 1.15) | – | 6-mm group: 91% (95% confidence interval: 0.836 to 0.998); 10-mm group: 100% | 6-mm group: −0.29 mm (IQR, −0.92 to 0.23); 10-mm group: −0.15 mm (IQR, −0.93 to 0.41) |
| Nunes et al. | 2016 | Clinical | 2.53±0.79 | 12.7 mm (range 11.94 to 19.99) | 100% | −0.67±0.63 mm |
| Pieri et al. | 2012 | Clinical | 1.94 ±0.46 (range 1.31 to 3.12) | 11.16±2.72 mm (range 7.42 to 17.34) | 96.8% | −0.60±0.13 mm |
| Ramaglia et al. | 2019 | Anatomical | 1.08 (C/I-R minimum value =0.58; C/I-R maximum value =2.25) | – | 100% | C/I-R ≤1: −0.653±0.58 mm; C/I-R >1: −0.287±0.26 mm |
| Rossi et al. | 2016 | Clinical | Test: 1.55 (1.02 to 2.53); Control: 0.97 (0.58 to 1.40) | Test: 7.7± 2.0 mm (4.5 to 12 mm); Control: 7.3± 1.9 mm (4.6 to 11 mm) |
Test: 86.7%; Control: 96.7% | Between the surgery and prosthesis delivery: Test: −0.38 mm; Control: −0.36 mm. After 5-year: Test: −0.14 mm; Control: −0.18 mm |
| Schneider et al. | 2012 | Clinical and anatomical | Anatomical: 1.04±0.26 (0.59 to 2.01); Clinical: 148±0.42 (0.82 to 3.24) | – | 95.8% | −0.008 mm (SD 0.74 mm) |
| Sharmann et al. | 2016 | Clinical | Test: 1.48±0.33; Control: 0.86±0.18 | – | Test 98%; Control 100% | Test: −0.19±0.62 mm; Control: −0.33±0.71 mm |
| Urdaneta | 2010 | Clinical | 1.6 (0.79 to 4.95) | 13 mm (8.5 to 26 mm) | 99.1% | 0.33 mm |
| Villarinho | 2017 | Clinical | 1.6±0.3 mm | 91.3% | 0.3±0.5 mm | |
| Zadeh | 2017 | Anatomical | Test: 1.78 (1.13 to 2.8); Control: 0.93 (0.59 to 1.39) | Test: 10.67 (6.8 to 16.8); Control: 10.19 (6.5 to 15.3) | Test: 96%; Control: 99% | Test: 0.04 mm; Control: −0.02 mm |
Table 2
| Article | Type of study | Follow-up | N° of patients and implants | Localization | Type of prosthesis | Type of implant | Length | Diameter |
|---|---|---|---|---|---|---|---|---|
| Anitua et al. | Retrospective | 23.18±7.7 months | 34 patients, 45 implants | Mandible | FDP | – | 5.5, 6.5 mm | 3,75, 4.0, 4.5, 5.0 mm |
| Birdi et al. | Retrospective | 20.9 months (range, 15.6–122.8 months) | 194 patients, 309 implants | Maxilla and mandible | Single crown | Bicon | 5.7, 6.0 mm | – |
| Blanes et al. | Perspective | 1 year | 83 patients, 192 implants | Posterior regions mandible and maxilla | Ceramic-to-metal fused fixed partial dentures or single crown | ITI | 8.01+−1.45 mm | – |
| Di Fiore et al. | Retrospective | 16 years (11–20 years) | 51 patients, 108 implants | Posterior mandible | 39 implants (36.1%) single crown; 69 implants (63.9%) multiple FDP | – | 7 mm | 3.75 mm (70.4%); 4.1 mm (29.6%) |
| Guljé et al. | Perspective | 12 months | 37 patients, 47 implants | Maxilla and mandible | Single crown | Astra Tech OsseoSpeed | 6 mm | 4 mm |
| Hadzik et al. | Perspective | 36 months | 30 patients, 30 implants | Maxilla | Cemented single crown | OsseoSpeed | 6 mm | 4 mm |
| Hingsammer et al. | Perspective | 20.52 months | 30 patients, 76 implants | Maxilla and mandible | Splinted crown | NobelSpeedy Groovy Shorty | 6.5 mm | 4 mm |
| Lee et al. | Retrospective | 5.7±2.0 years | 259 patients, 175 implants | Maxilla and mandible | 137 single crowns, 122 splinted crowns | 3 different implant systems | – | – |
| Malchiodi et al. | Perspective | 3 years | 151 patients, 280 implants | Maxilla and mandible | 102 single crown; 157 FPDs | – | 5 mm (27.0%); 7 mm (31.3%); 9 mm (34.0%); 12 mm (7.7%) | 4.1 mm (60.6%); 5 mm (39.4%) |
| Mangano et al. | Perspective | 5 years | 50 patients, 68 implants | Maxilla and mandible | 49 single crowns; 9 FDP | Leone | 6.5 mm | 5 mm |
| Naenni et al. | Perspective | 5±0.7 years | 96 patients (86 after 5 years), 96 implants | Maxilla and mandible | Single crown | Standard Plus Tissue Level Implant (Straumann) | Case: 6 mm; Control: 10 mm | 4.1 mm |
| Nunes et al. | Retrospective | 36 months | 59 patients, 118 implants | Maxilla and mandible | 28 single crown; 90 splinted crowns | – | 7 mm | 4 mm |
| Pieri et al. | Perspective | 2 years | 25 patients, 61 implants | Mandible | FDP | OsseoSpeed (Astra Tech) | 6 mm | 4 mm |
| Ramaglia et al. | Perspective | 5 years | 78 implants | Mandible and maxilla | Metal ceramic crown | – | <10-mm long: 35 implants; ≥10-mm long (from 10 to 15 mm): 43 implants | – |
| Rossi et al. | Perspective | 5 years | 45 patients, 30 test implants, 30 control implants | Maxilla and mandible | – | Straumann AG, with a SLA modified surface | Case: 6 mm; Control: 10 mm | 4.1 mm |
| Schneider et al. | Retrospective | 6.2 years (4.73 to 11.7 years) | 70 patients, 100 implants | Maxilla and mandible | Single crown | 24 Straumann, 76 Branemark | 11.5 mm (7 to 15 mm) | 3.75–4.1 mm: 66%; 4.8–5 mm: 34% |
| Sharmann et al. | Perspective | 36 months | 47 control implants, 47 test implants | Maxilla and mandible | Single crown | Straumann | Case: 6 mm; Control: 10 mm | 4.1 mm |
| Urdaneta et al. | Retrospective | 70.7±23 months | 81 patients, 326 implants | Maxilla and mandible | Single crown | Bicon | 6 mm; 8 mm; 11 mm; 14 mm | 3.5 mm; 4 mm; 4.5 mm; 5 mm; 6 mm |
| Villarinho et al. | Perspective | 45±9 months | 20 patients, 46 implants | Maxilla and mandible | Single Crown | Straumann Standard Plus | 6 mm | 4.1 mm |
| Zadeh et al. | Perspective | 3 years | 95 patients, 209 implants | Maxilla and mandible | FDPs | OsseoSpeed | Test 6 mm; Control 11 mm | 4 mm |
Biomechanically, unfavourable ratio may influence marginal bone through the lever mechanism. When subjected to lateral forces, implant restorations with long lever arm generate greater stress at the bone crest. It has been demonstrated in a cantilever model that crown height increased from 10 to 20 mm, lead to a proportional moment increment (34). C/I-R is calculated as the ratio between the crown and implant lengths. We can distinguish two different C/I-R:
- Anatomical ratio is the ratio between the distance from the apex to the shoulder of the implant, and the distance from the shoulder of the implant to the end of the crown;
- Clinical ratio is the ratio between the distance from the apex to the bone level, and the distance from the bone level to the end of the crown.
Clinical ratio is considered a more accurate since the implant-bone interface is less rigid than the connection at the implant shoulder, due to bone viscoelasticity (16). Among the studies included in this review, many concluded that the relationship between C/I-R and MBL is not significant. Urdaneta et al. (31) concluded that larger CI ratio led to an increase in prosthetic complications but had no significant influence on MBL. In this study 16% of the sample had CI ratio >2. Nunes et al. (25) found a weak inverse correlation between CI ratio and MBL. Blanes et al. (16) stated that there were no statistical relationship between CI ratio and MBL. Birdi et al. (15) found no significant relationship between CI ratio and first bone-to-implant contact levels. Schneider et al. (29) concluded that technical and biological CI ratio had no significant correlation on the MBL, technical and biological complications and implant survival. Mangano et al. (23) found no correlation between MBL and CI ratio along time, with a 0.023 mm increase in 1-year bone resorption for every 0.1 increase in CI ratio. However, other studies found a stronger correlation between C/I-R and MBL. Di Fiore et al. (17) showed that, at multivariable analysis, C/I-R >2 was correlated with higher MBL. It was estimated that C/I-R >2 led to an increase of 0.28 mm in MBL. However, the authors underlined that this increment could be considered clinically irrelevant. Hingsammer et al. (20) concluded that a MBL of 0.71 mm is considered to be satisfactory and a C/I-R of 1.7 can be considered as a threshold to avoid early marginal bone changes. Malchiodi et al. (22) showed that implants with C/I ratio >2 had a MBL of 0.72 mm. Statistical analysis revealed that both anatomical and clinical CI ratio had a correlation with MBL. The authors concluded that, from a biomechanical point of view, to avoid excessive bone loss, anatomical and clinical C/I ratio should not exceed respectively 3.1 and 3.4. It was seen that C/I ratio resulted the main factor correlated to implant success and crestal bone loss.
The difference between all this findings can be found in various aspects. Many studies mixed together implants of different lengths; moreover, the definition of short implant is not standardized. Tawil and Younan considered short an implant <10 mm (35). Nisand and Renouard defined “short” implants with a length of <8 mm and extra-short the one <5 mm (36). Since the length of the implant seems not to be correlated to the lever mechanism, the portion that may be significantly correlated is the crown. In many of the previous mentioned studies, the crown-height-space was not considered in relation to CI ratio. Anitua et al. (14) analysed 45 extra-short implants with a mean CI ratio of 2.4 and a mean CHS of 17.05. Results showed that implants with MBL <2 mm had a mean CHS of 17 mm, while implants with MBL >2 had a mean CHS of 21 mm. Statistical analyses revealed that CHS had a positive correlation with bone loss. Nissan et al. (37) in an in vitro study showed that an increased crown height from 6 to 12 mm, in case of off-axis loading of 30 degrees determined a proportional increase stress distribution (17.72 vs. 30.09 MPa). CHS higher than 15 mm is considered as biomechanically unfavourable, resulting in increased stress at bone level. Failure were noted at CHS >15 mm and CI ratio at 1.75 when force application was at 30 degrees. The authors concluded that CHS is more significant than CI ratio in the evaluation of the adverse effects related to biomechanics, and studies about the effects of C/I ratio should mention both implant length and CHS in their results.
In this review was considered both splinted and unsplinted implants. Many studies underline that splinting crowns together could better distribute non-axial forces, minimizing their load to the restoration and bone, and increasing the load area (7). Moreover, splinting is recommended in case of poor quality bone to be reduced the marginal bone stress under horizontal load (38). Therefore, splint implants could alter the real impact of C/I-R on MBL resulting in less cervical stress for a better forces distribution. However, in an in vitro study Nissan et al. (37) proved the splinting implants can result in greater crestal bone loss.
In conclusion, according to a recent consensus of EAO (39), is possible to state that crown-to-implant not exceed 2.2 did not influence the possibility of biological complications and lead to a not significant MBL. Further research should investigate the complications of higher ratios, the implications of splinted implants on forces distribution and the role of crown height on MBL.
Acknowledgments
Funding: None
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://fomm.amegroups.org/article/view/10.21037/fomm-20-57/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.org/article/view/10.21037/fomm-20-57/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Papaspyridakos P, Bordin TB, Natto ZS, et al. Complications and survival rates of 55 metal-ceramic implant-supported fixed complete-arch prostheses: A cohort study with mean 5-year follow-up. J Prosthet Dent 2019;122:441-9. [Crossref] [PubMed]
- Pjetursson BE, Thoma D, Jung R, et al. A systematic review of the survival and complication rates of implant-supported fixed dental prostheses (FDPs) after a mean observation period of at least 5 years. Clin Oral Implants Res 2012;23:22-38. [Crossref] [PubMed]
- Papaspyridakos P, Chen CJ, Singh M, et al. Success Criteria in Implant Dentistry: A Systematic Review. J Dent Res 2012;91:242-8. [Crossref] [PubMed]
- Simons WF, De Smit M, Duyck J, et al. The proportion of cancellous bone as predictive factor for early marginal bone loss around implants in the posterior part of the mandible. Clin Oral Implants Res 2015;26:1051-9. [Crossref] [PubMed]
- Rangert B, Krogh PH, Langer B, Van Roekel N. Bending overload and implant fracture: a retrospective clinical analysis. Int J Oral Maxillofac Implants 1995;10:326-34. [PubMed]
- Brunski JB, Puleo DA, Nanci A. Biomaterials and biomechanics of oral and maxillofacial implants: current status and future developments. Int J Oral Maxillofac Implants 2000;15:15-46. [PubMed]
- Kim Y, Oh TJ, Misch CE, et al. Occlusal considerations in implant therapy: clinical guidelines with biomechanical rationale: Occlusal consideration in implant therapy. Clin Oral Implants Res 2005;16:26-35. [Crossref] [PubMed]
- Zurdo J, Romão C, Wennström JL. Survival and complication rates of implant-supported fixed partial dentures with cantilevers: a systematic review. Clin Oral Implants Res 2009;20:59-66. [Crossref] [PubMed]
- Leung KC, Chow TW, Wat PY, et al. Peri-implant bone loss: management of a patient. Int J Oral Maxillofac Implants 2001;16:273-7. [PubMed]
- Ozgur GO, Kazancioglu HO, Demirtas N, et al. Risk factors associated with implant marginal bone loss: a retrospective 6-year follow-up study. Implant Dent 2016;25:122-7. [Crossref] [PubMed]
- Tawil G, Aboujaoude N, Younan R. Influence of prosthetic parameters on the survival and complication rates of short implants. Int J Oral Maxillofac Implants 2006;21:275-82. [PubMed]
- Quaranta A, Piemontese M, Rappelli G, et al. Technical and biological complications related to crown to implant ratio: a systematic review. Implant Dent 2014;23:180-7. [Crossref] [PubMed]
- Garaicoa-Pazmiño C, Suárez-López del Amo F, Monje A, et al. Influence of crown/implant ratio on marginal bone loss: a systematic review. J Periodontol 2014;85:1214-21. [Crossref] [PubMed]
- Anitua E, Alkhraist M, Piñas L, et al. Implant Survival and Crestal Bone Loss Around Extra-Short Implants Supporting a Fixed Denture: The Effect of Crown Height Space, Crown-to-Implant Ratio, and Offset Placement of the Prosthesis. Int J Oral Maxillofac Implants 2014;29:682-9. [Crossref] [PubMed]
- Birdi H, Schulte J, Kovacs A, et al. Crown-to-Implant Ratios of Short-Length Implants. Journal of Oral Implantology 2010;36:425-33. [Crossref] [PubMed]
- Blanes RJ, Bernard JP, Blanes ZM, et al. A 10-year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin Oral Implants Res 2007;18:707-14. [Crossref] [PubMed]
- Di Fiore A, Vigolo P, Sivolella S, et al. Influence of Crown-to-Implant Ratio on Long-Term Marginal Bone Loss Around Short Implants. Int J Oral Maxillofac Implants 2019;34:992-8. [Crossref] [PubMed]
- Guljé FL, Raghoebar GM, Erkens WA, et al. Impact of Crown-Implant Ratio of Single Restorations Supported by 6-mm Implants: A Short-Term Case Series Study. Int J Oral Maxillofac Implants 2016;31:672-5. [Crossref] [PubMed]
- Hadzik J, Krawiec M, Sławecki K, et al. The Influence of the Crown-Implant Ratio on the Crestal Bone Level and Implant Secondary Stability: 36-Month Clinical Study. Biomed Res Int 2018;2018:4246874. [Crossref] [PubMed]
- Hingsammer L, Watzek G, Pommer B. The influence of crown-to-implant ratio on marginal bone levels around splinted short dental implants: A radiological and clinical short term analysis. Clin Implant Dent Relat Res 2017;19:1090-8. [Crossref] [PubMed]
- Lee KJ, Kim YG, Park JW, et al. Influence of crown-to-implant ratio on peri-implant marginal bone loss in the posterior region: a five-year retrospective study. J Periodontal Implant Sci 2012;42:231. [Crossref] [PubMed]
- Malchiodi L, Cucchi A, Ghensi P, et al. Influence of crown-implant ratio on implant success rates and crestal bone levels: a 36-month follow-up prospective study. Clin Oral Implants Res 2014;25:240-51. [Crossref] [PubMed]
- Mangano F, Frezzato I, Frezzato A, et al. The Effect of Crown-to-Implant Ratio on the Clinical Performance of Extra-Short Locking-Taper Implants. J Craniofac Surg 2016;27:675-81. [Crossref] [PubMed]
- Naenni N, Sahrmann P, Schmidlin PR, et al. five-year survival of short single-tooth implants (6 mm): a randomized controlled clinical trial. J Dent Res 2018;97:887-92. [Crossref] [PubMed]
- Nunes M, Almeida R, Felino A, et al. The Influence of Crown-to-Implant Ratio on Short Implant Marginal Bone Loss. Int J Oral Maxillofac Implants 2016;31:1156-63. [Crossref] [PubMed]
- Pieri F, Aldini NN, Fini M, et al. Preliminary 2-year report on treatment outcomes for 6-mm-long implants in posterior atrophic mandibles. Int J Prosthodont 2012;25:279-89. [PubMed]
- Ramaglia L, Di Spirito F, Sirignano M, et al. A 5-year longitudinal cohort study on crown to implant ratio effect on marginal bone level in single implants. Clin Implant Dent Relat Res 2019;21:916-22. [Crossref] [PubMed]
- Rossi F, Botticelli D, Cesaretti G, et al. Use of short implants (6 mm) in a single-tooth replacement: a 5-year follow-up prospective randomized controlled multicenter clinical study. Clin Oral Implants Res 2016;27:458-64. [Crossref] [PubMed]
- Schneider D, Witt L, Hämmerle CHF. Influence of the crown-to-implant length ratio on the clinical performance of implants supporting single crown restorations: a cross-sectional retrospective 5-year investigation: Influence of the c/i ratio on the performance of implants supporting single crown restorations. Clin Oral Implants Res 2012;23:169-74. [Crossref] [PubMed]
- Sahrmann P, Naenni N, Jung RE, et al. Success of 6-mm Implants with Single-Tooth Restorations: A 3-year Randomized Controlled Clinical Trial. J Dent Res 2016;95:623-8. [Crossref] [PubMed]
- Urdaneta RA, Rodriguez S, McNeil DC, et al. The effect of increased crown-to-implant ratio on single-tooth locking-taper implants. Int J Oral Maxillofac Implants 2010;25:729-43. [PubMed]
- Villarinho EA, Triches DF, Alonso FR, et al. Clin Implant Dent Relat Res 2017;19:671-80. [Crossref] [PubMed]
- Zadeh HH, Guljé F, Palmer PJ, et al. Marginal bone level and survival of short and standard-length implants after 3 years: An Open Multi-Center Randomized Controlled Clinical Trial. Clin Oral Implants Res 2018;29:894-906. [Crossref] [PubMed]
- Misch CE, Goodacre CJ, Finley JM, et al. Consensus conference panel report: crown-height space guidelines for implant dentistry-part 2. Implant Dent 2006;15:113-21. [Crossref] [PubMed]
- Tawil G, Younan R. Clinical evaluation of short, machined-surface implants followed for 12 to 92 months. Int J Oral Maxillofac Implants 2003;18:894-901. [PubMed]
- Nisand D, Renouard F. Short implant in limited bone volume. Periodontol 2000 2014;66:72-96. [Crossref] [PubMed]
- Nissan J, Gross O, Ghelfan O, et al. The Effect of Splinting Implant-Supported Restorations on Stress Distribution of Different Crown-Implant Ratios and Crown Height Spaces. J Oral Maxillofac Surg 2011;69:2990-4. [Crossref] [PubMed]
- Wang TM, Leu LJ, Wang J, et al. Effects of prosthesis materials and prosthesis splinting on peri-implant bone stress around implants in poor-quality bone: a numeric analysis. Int J Oral Maxillofac Implants 2002;17:231-7. [PubMed]
- Hämmerle CHF, Cordaro L, Alccayhuaman KAA, et al. Biomechanical aspects: Summary and consensus statements of group 4. The 5th EAO Consensus Conference 2018. Clin Oral Implants Res 2018;29:326-31. [Crossref] [PubMed]
Cite this article as: Di Fiore A, Maniero F, Stellini E. The influence of crown-to-implant ratio on marginal bone loss: a narrative review. Front Oral Maxillofac Med 2020;2:29.