
Vertebral metastasis from squamous cell carcinoma of the tongue
Tongue squamous cell carcinoma represents the most frequent and aggressive cancer of the oral cavity. It usually metastasizes via the lymphatic system at cervical level and distant metastases are uncommon. In case of metastasis outside the neck, the lung is the organ most frequently affected (1). In contrast, vertebral metastases are extremely rare. Approximatively, 7 cases of squamous cell carcinoma of tongue with spinal metastases have been described (2). The most common symptom related with vertebral metastases is the pain described as progressive and unremitting. Moreover, it is worse at night and usually improves with activity and anti-inflammatory medication (3). Motor and sensory dysfunctions are also common with the progressive spinal infiltration. X-ray, CT scan, PET and MRI are useful to confirm the lesion in case of suspicious. The treatment aims to reduce neurological disability and pain. According with literature, radiotherapy, palliative CT, decompressive surgery and steroids may be useful to manage this complication (4).
We report three cases of vertebral metastases in patients affected by squamous cell carcinoma of the oral tongue. Two of these patients were males of 36 and 43 years old respectively (Patient 1 and 2), and the third was a female of 79 years old (Patient 3). All patients presented a positive biopsy for squamous cell carcinoma of the tongue before surgery and all of them underwent tumorectomy of the primary tumor and neck dissection. Interestingly, only one of these patients (patient 2) presented the common risk factors for squamous cell carcinoma of the oral cavity (alcohol and tobacco). According with the postoperative pathological findings the patients were staged as T2N1M0 (DOI 0.9 cm) (patient 1), T3N2aM0 (DOI 1.3 cm) (patient 2) and T1N2aM0 (DOI 0.4 cm) (patient 3) with free surgical margins. The clinical stage of the primary tumor was established following the recommendations of the International Union Against Cancer 8th edition (UICC) (5).
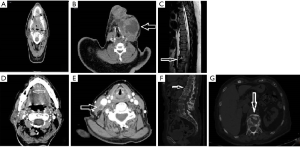
Interestingly, patient 1 showed an isolated cervical metastasis at level IV after postoperative pathological examination. In contrast, patient 2 and 3 both showed two infiltrated cervical nodes at level II and III. Thus, all patients were secondarily treated with adjuvant RT. However, all cases presented a no operable cervical relapse during the first 12 months of follow-up and were consequently treated with adjuvant CT (Figure 1). Despite the treatment, vertebral metastases were successively evidenced in all patients during the first 21 months after primary surgery. Particularly, patient 1 and 3 showed a spine metastasis affecting T12. On the other hand, the spine metastasis experienced by patient 2 affected L1. All metastases were diagnosed with a X-ray and confirmed by MRI or CT scan. Histopathological confirmation was obtained only for patient 1. All patients reported an intensive and progressive pain at the beginning. Motor and sensory disability also appeared in all patients in days or weeks. The treatment was focused on the treatment of pain and neurological complications. Steroids and opioids were used in all cases. Moreover, patient 1 was also treated with palliative decompressive surgery to reduce intractable pain. Unfortunately, all patients died approximatively 1 month after diagnosis.
Interestingly, all metastasis registered in our series were caused by small cancer with a high tendency to metastasize (one T1 and one T2 tumor). Indeed, all cases showed cervical involvement after postoperative pathological analysis and all patients suffered an inoperable cervical recurrence during follow-up. Hence, the ability to affect the spine would be an intrinsic feature of the tumor unrelated to the size of the lesion. This data is comparable with the outcome of other studies (2). Vertebral metastases represent an extremely poor prognostic sign and all cases reported in literature died between 2 weeks and 3 months after diagnosis (1,6).
To summarize, our report contains three central points. First, spinal metastases represent a sign of very poor prognosis in patients with squamous cell carcinoma of the tongue. Second, this complication should be suspected in case of localized bone pain in patients with advanced tongue cancers. The establishment of a palliative treatment is essential to try to maintain an acceptable quality of life during the last phases of the disease. Third, the ability to cause spinal metastasis may be a feature unrelated to the size of the primary lesion.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://fomm.amegroups.org/article/view/10.21037/fomm-20-18/coif). PC serves as an unpaid editorial board member of Frontiers of Oral and Maxillofacial Medicine from Apr 2020 - Mar 2022. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Carlson ER, Ord RA. Vertebral metastases from oral squamous cell carcinoma. J Oral Maxillofac Surg 2002;60:858-62. [Crossref] [PubMed]
- Trilling GM, Cho H, Ugas MA, et al. Spinal metastasis in head and neck cancer. Head Neck Oncol 2012;4:36. [Crossref] [PubMed]
- Harel R, Angelov L. Spine metastases: current treatments and future directions. Eur J Cancer 2010;46:2696-707. [Crossref] [PubMed]
- Sciubba DM, Petteys RJ, Dekutoski MB, et al. Diagnosis and management of metastatic spine disease. A review. J Neurosurg Spine 2010;13:94-108. [Crossref] [PubMed]
- Lydiatt WM, Patel SG, O'Sullivan B, et al. Head and Neck cancers-major changes in the American Joint Committee on cancer eighth edition cancer staging manual. CA Cancer J Clin 2017;67:122-37.
- Preciado DA, Sebring LA, Adams GL. Treatment of patients with spinal metastases from head and neck neoplasms. Arch Otolaryngol Head Neck Surg 2002;128:539-43. [Crossref] [PubMed]
Cite this article as: Cariati P, Pampin Ozan D, Arroyo Rodriguez S. Vertebral metastasis from squamous cell carcinoma of the tongue. Front Oral Maxillofac Med 2020;2:8.

